Do you know about the 11 common fundus diseases?
Take a picture of your fundus to detect eye diseases early!
From a few years ago to now, the theme of Eye Care Day has been calling on people to check their fundus regularly. But when they really go for a check-up and the results come out, looking at the “orange ping-pong ball” on the image, their little heads are filled with big question marks.
What is this? Am I sick or not?
Don’t panic, here are the fundus photos of 11 common eye diseases. You can tell if you have the disease or not just by looking at them!
When it comes to the commonly used term “fundus” in ophthalmology, many non-medical professionals think that it is under the eyeball. In fact, it is not. So where is the fundus? The fundus is actually the tissue at the back of the eyeball, that is, the inner membrane of the eyeball – the retina, the optic disc, the macula, and the central retinal artery and vein.
With the improvement of public medical professional knowledge, fundus diseases have become more and more familiar to everyone. Among them, fundus photography, optical coherence tomography (OCT), and ophthalmic B-ultrasound are all commonly used methods for examining fundus diseases.
What is the fundus?
The fundus commonly referred to clinically refers to the internal structure of the eyeball from the lens to the back, including the retina, fundus blood vessels, optic nerve head, optic nerve fibers, macula on the retina, and choroid behind the retina.
The fundus is filled with abundant blood vessels and nerves, and involves many parts of the body, so the diseases related to it are also more numerous and complex, and most fundus diseases cause serious damage to visual function.
Among them, the macular area on the retina is a high-incidence area for many fundus diseases. It is the place where the eye’s vision is relatively sharp and is responsible for collecting a large amount of visual information. If it has pathological changes such as bleeding, proliferation, and exudation, it may cause a significant decrease in vision.
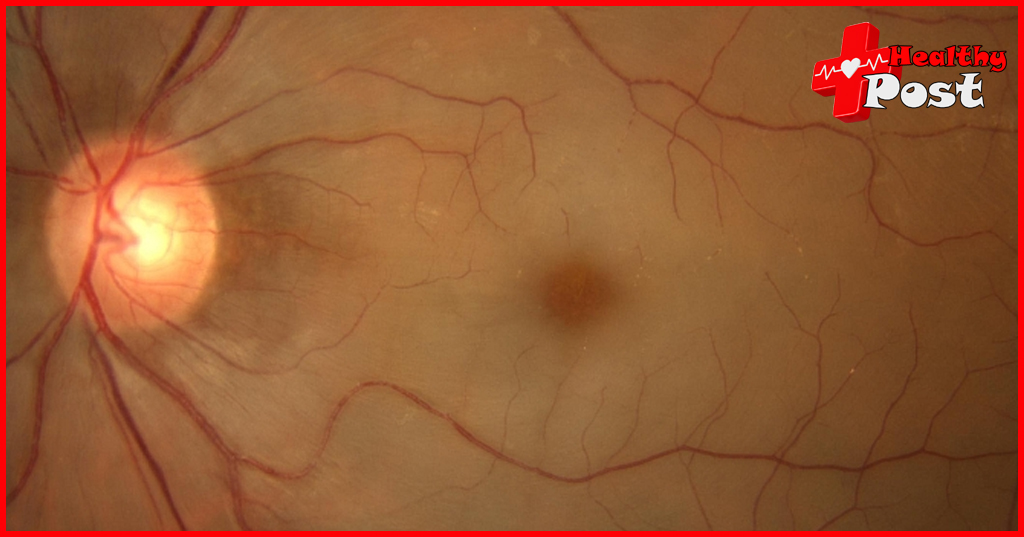
This is a normal color photograph of the posterior pole fundus and OCT image of the macular area.
Fundus color photo: various tissue structures in the posterior pole of the fundus
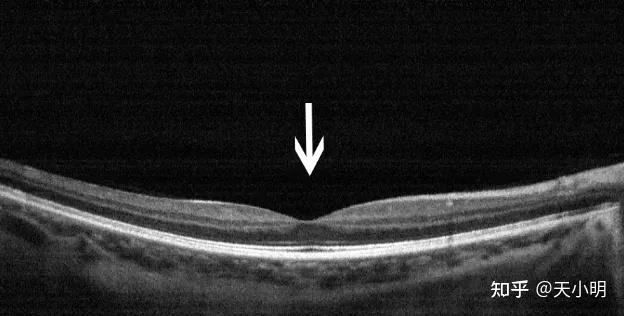
OCT: cross-section of the retina in the macular area, with the depression being the fovea
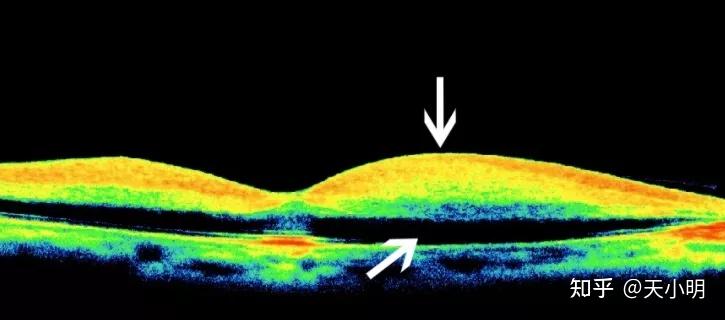
01 Central serous chorioretinopathy

Central serous chorioretinopathy, also known as “central serous chorioretinopathy”, is a serous detachment of the retina in the macula. The area of pigment epithelial detachment may be very small and difficult to detect. This disease is more common in young and middle-aged men, and patients may experience symptoms such as decreased vision and darkening of vision. Because this disease is a self-limiting disease, most patients can recover on their own, but it is easy to relapse and the prognosis is generally good.
Fundus color photo: The color of the macula becomes darker, and the fovea is red with a halo around it
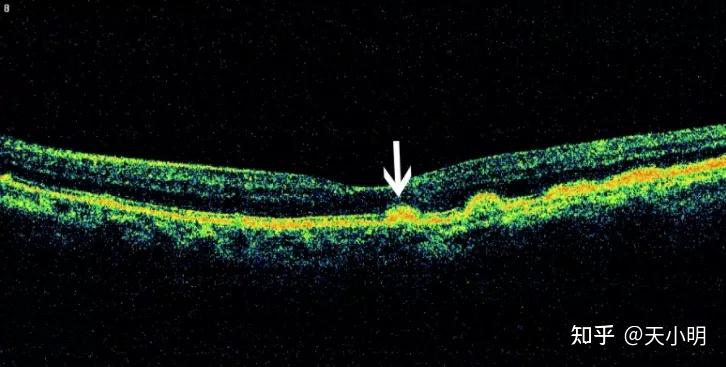
OCT: The macular edema area is a colored triangle
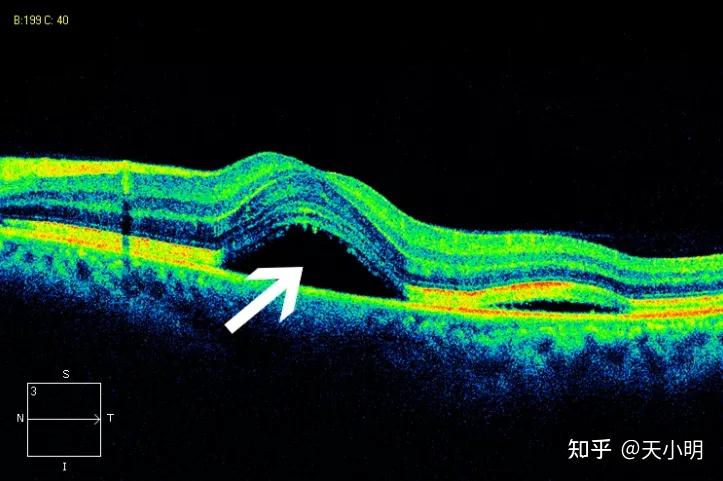
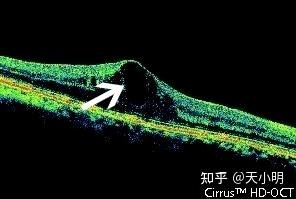
02 Macular hole (full thickness)
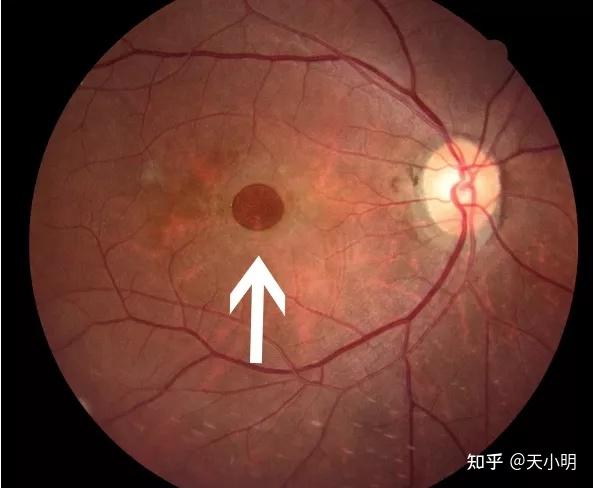
Macular hole, which is commonly referred to as “a hole in the fundus” or “a tear in the retinal membrane”, refers to the tissue defect from the inner limiting membrane of the retina to the photoreceptor cell layer in the macula, which seriously damages the patient’s central vision.
Fundus color photo: macular hole, red and round
OCT: There is no tissue or light reflection at the hole, and it appears black
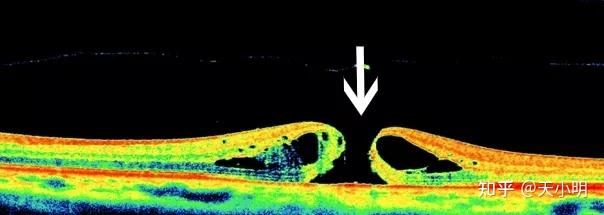
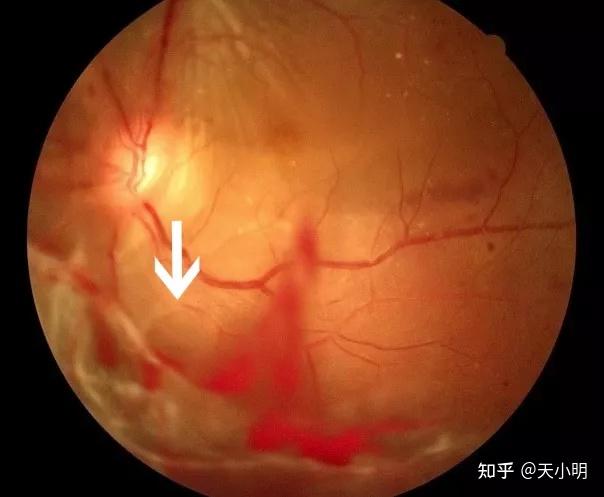
03 Central retinal vein occlusion
Central retinal vein occlusion is a disease caused by systemic diseases such as hypertension, atherosclerosis, diabetes, etc., which cause the inner wall of the blood vessels to thicken and roughen, resulting in slowed blood flow or stasis, forming blood clots to block the blood vessels; or due to other reasons that cause high blood concentration, or due to low blood pressure, causing slow blood flow and causing blood clots, resulting in sudden vision loss.
Fundus color photo: retinal flame hemorrhage
OCT: Cystoid edema in the macular area, the edema area appears as a black triangle
04 Central retinal artery occlusion
Central retinal artery occlusion is also known as “eye stroke”. It is mostly caused by changes in the blood vessel wall such as vascular embolism, arterial spasm, atherosclerosis or endarteritis, thrombosis, or external compression of blood vessels. The main manifestation is a sudden and sharp decrease in vision in one eye, or even loss of light perception.
Once the disease occurs, it needs to be treated as soon as possible, but most patients have already lost the chance of rescue by the time they seek medical treatment, so the prognosis of this disease is usually poor.
Fundus color photo: the fundus is grayish yellow, and the macular area is cherry red
OCT: The retinal nerve fiber layer is red and yellow with high reflection (middle arrow), and the edema underneath is obscured by dark areas (short arrows).
05 Diabetic retinopathy-non-proliferative stage

Non-proliferative diabetic retinopathy refers to the absence of new blood vessels and proliferative membranes, and is mainly manifested by symptoms such as bleeding, exudation, ischemia, and edema. During treatment, panretinal photocoagulation can be performed for patients with severe non-proliferative diabetic retinopathy, and anti-VEGF treatment can also be considered for patients with macular edema.
Fundus color photo: yellow-white exudation in the macular area of the fundus, and many retinal hemorrhages
OCT: Cystoid edema in the macular area, the edema area appears as a black oval
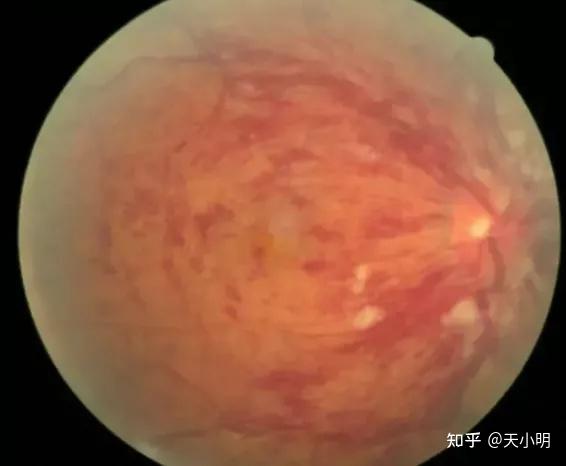
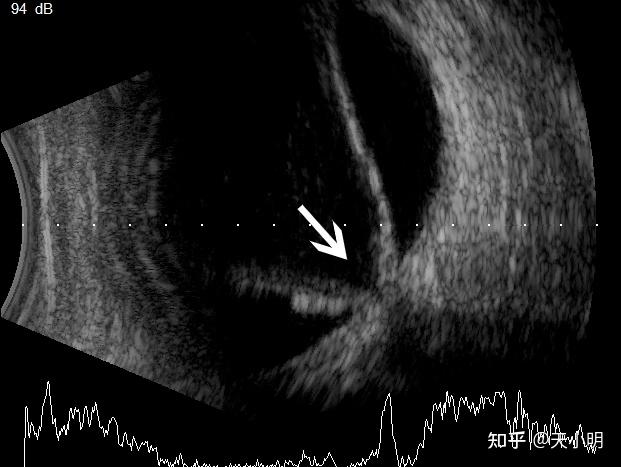
06 Diabetic Retinopathy-Proliferative Phase
Proliferative diabetic retinopathy is a type of diabetic complication. When the blood sugar of diabetic patients cannot be controll for a long time, the condition worsens and causes retinopathy. Proliferative diabetic retinopathy may be cause by ocular hypoxia and ischemia due to increased blood sugar.
This disease is quite serious and requires timely surgical treatment and timely control of diabetes complications. Usually, diabetes is controll and patients with diabetes need to inject insulin regularly. Try to avoid diabetes complications.
Fundus color photo: Hemorrhage and white translucent fibroproliferative membrane can be see in the vitreous
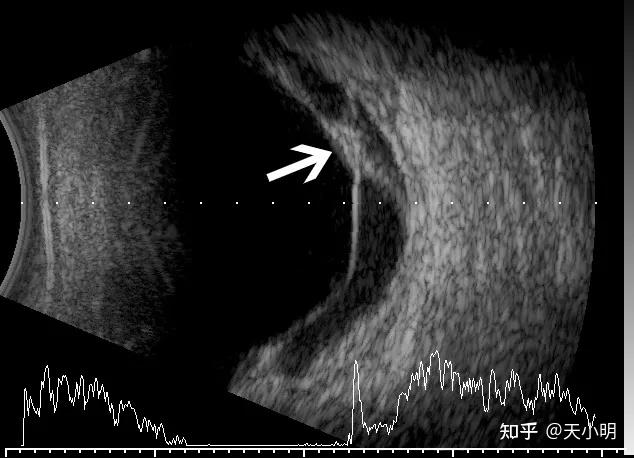
Ultrasound: Vitreous blood accumulation, accompanied by local tractional retinal detachment, presenting a “trapezoidal bench shape”
07 Vitreous hemorrhage
Vitreous hemorrhage is a common complication of eye trauma or retinal vascular disease that causes visual impairment. Hemorrhage not only makes the refractive medium turbid, but also can cause serious damage to eye tissues;
A small amount of bleeding may cause floaters or red flocculent floating objects;
When there is heavy bleeding, there may be a large number of red blood cells or blood clots in the vitreous. There are many causes of this disease, including eye trauma, diabetes, surgery, and spontaneous. The treatment of vitreous hemorrhage is mainly through drugs, surgery and other methods.
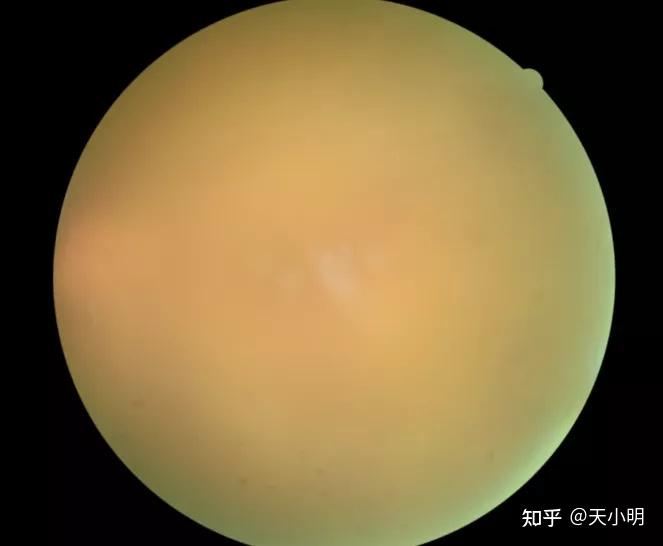
Fundus color photo: turbidity
Ultrasound: The blood in the vitreous body is diffuse, dense and medium echo points
08 Age-related macular degeneration (dry form)

It mostly occurs in the elderly over 50 years old. The onset is slow, and the patient’s vision deteriorates unknowingly. Visual distortion may occur, and the degree of vision loss is similar in both eyes.
In the early stage of the disease, yellow-white circular drusen of varying sizes can be see in the posterior pole of the fundus. Which can fuse, with hyperplasia or atrophy of the pigment epithelium, disappearance of foveal light reflex, and disordered pigmentation in the posterior pole, and further appearance of a clearly demarcated map-like atrophy area. In the late stage, the choroidal capillaries in this area atrophy, and expose choroidal large vessels can be see.
Fundus color photo: a large number of drusen in the fundus, appearing as small golden dots
OCT: Drusen appear as small arch-shaped protrusions, small red arches
09 Age-related macular degeneration (wet)

Wet macular degeneration is manifest by sudden monocular vision loss, visual distortion or central dark spots, and the other eye may develop symptoms after a long time. Subretinal hemorrhage and exudation in the posterior pole of the fundus, sometimes with gray-yellow lesions, may be new blood vessels.
Fundus color photo: hemorrhage in the macular area, with yellow-white surrounding hemorrhage
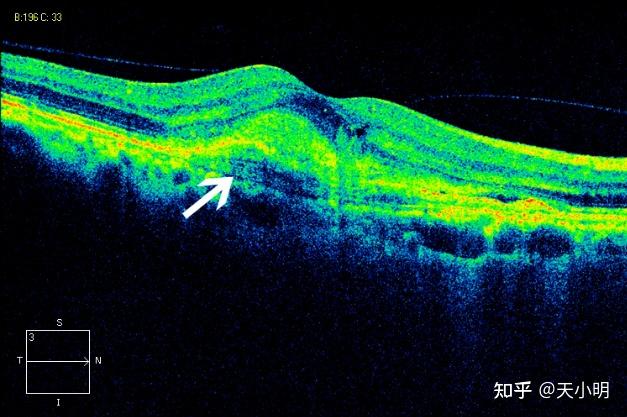
OCT: The neuroepithelium in the macular area is slightly raise, with yellow, highly reflective hemorrhages and new blood vessels underneath, which are spindle-shape
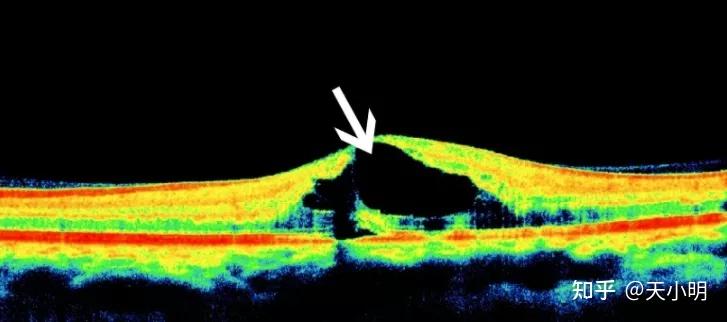
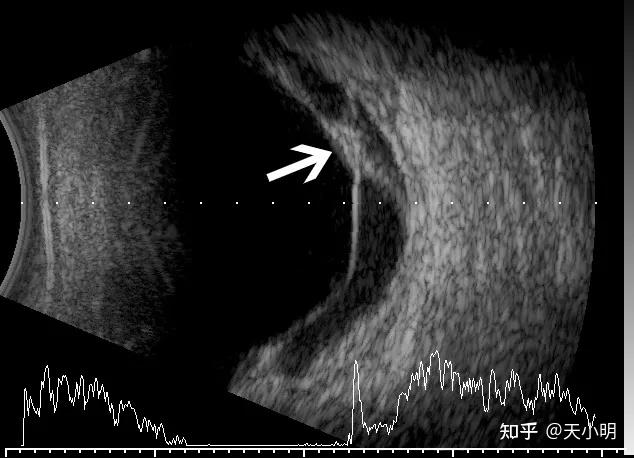
10. Retinal detachment
Retinal detachment is a more serious and common blinding eye disease. The retina is a translucent membrane in the eye, an important tissue that senses external light information. It is located at the bottom of the eyeball and has a very fine network structure and rich metabolic and physiological functions. The retina is divide into ten layers, nine of which are neuroepithelial layers, which are the photosensitive layer of the eye. Outside the neuroepithelial layer is the pigment epithelium, and there is a potential gap between the two layers.
Retinal detachment is the separation of the retinal neuroepithelium and the pigment epithelium. After retinal detachment, the choroidal blood supply is lost, and the pigment epithelium is prone to become free and atrophy. If it is not reset and restore in time, vision will not be easy to recover.
Fundus color photo: The upper retina is detached, the fundus color is lighter than the lower one, and there are wrinkles
Ultrasound: The detached retina is connect to the optic nerve and presents a “funnel-shaped V”
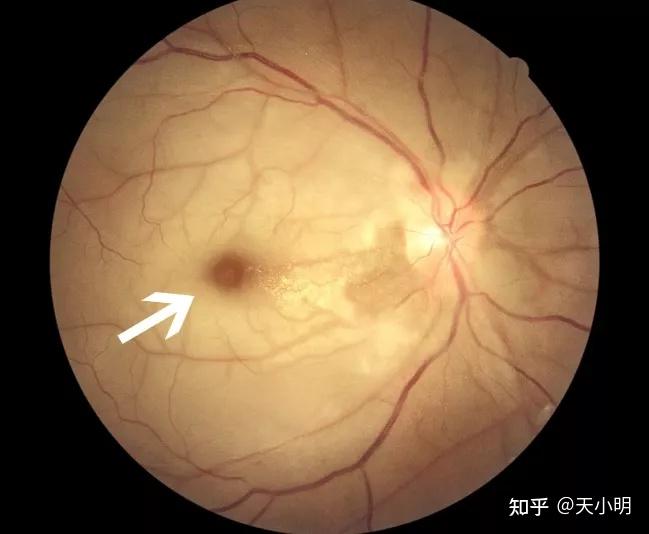
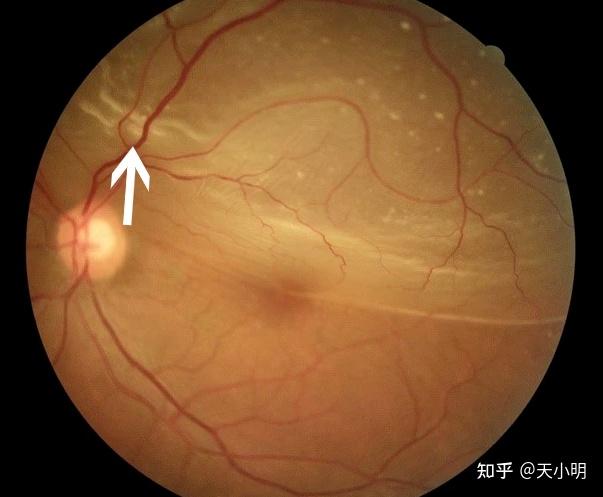
11 High myopia fundus lesions combined with choroidal neovascularization

Choroidal neovascularization refers to the proliferation of blood vessels from choroidal capillaries, which expand through the rupture of Bruch’s membrane and proliferate between Bruch’s membrane and retinal pigment epithelium, or between neural retina and retinal pigment epithelium, or between retinal pigment epithelium and choroid. Many diseases involving RPE-Bruch’s membrane-choroidal capillaries complex can lead to the formation of CNV, also known as subretinal neovascularization. It is more common in the macula, thus impairing central vision.
This disease has become one of the main causes of blindness. It is common in adult eyes, especially those over 60 years old. It should be discover early and treat in time.

Fundus color photo: leopard-like fundus, hemorrhage in the macular area, and yellow-white surroundings of the hemorrhage
OCT: Choroidal neovascularization in the macular area appears as a small raised bulge
Note: In this article all images are from chinese network.
