Diagnosis and treatment of hydrocephalus in children
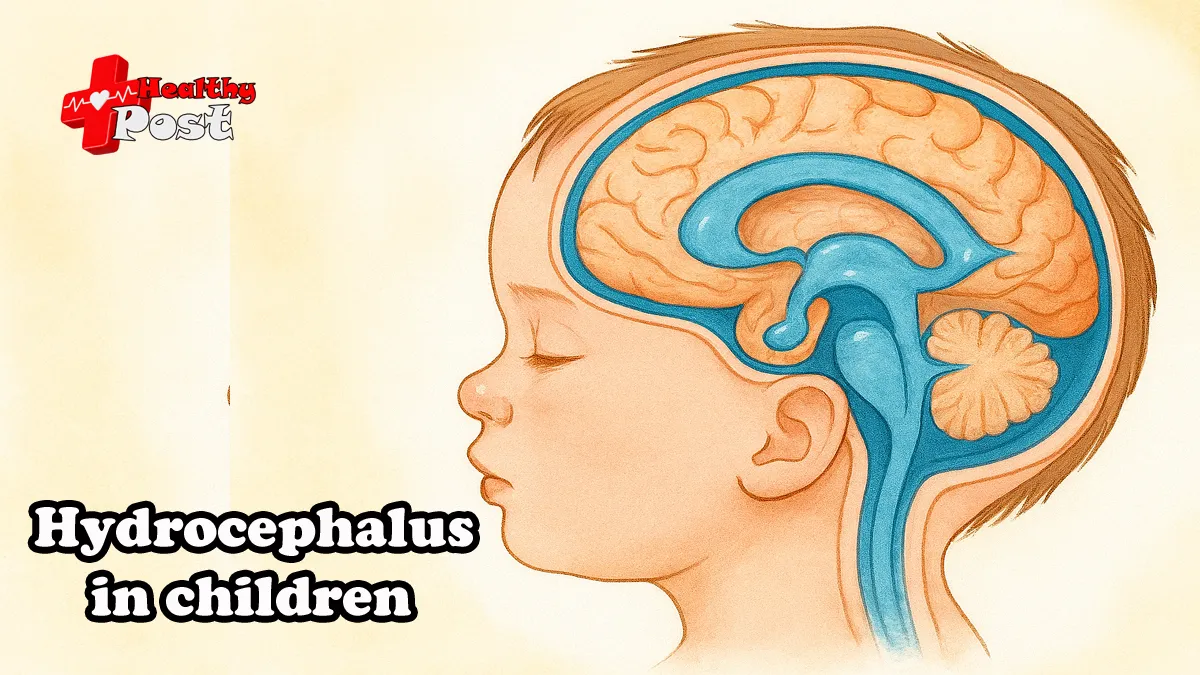
Hydrocephalus is a disease characterized by an increase in cerebrospinal fluid volume, leading to increased intracranial pressure. Clinically, it is characterized by an enlarged head, open anterior fontanelle, and separation of cranial sutures. Based on the location of the cerebrospinal fluid circulation obstruction. It can be divide into two types: non-communicating (obstructive) and communicating. In the former, the cerebrospinal fluid is obstruct above the foramen of the fourth ventricle. While in the latter, it is obstruct below the foramen of the fourth ventricle. This disease is most common in children age 6 months to 7 years. During the progression of the disease, children with hydrocephalus often experience irritability, lethargy, loss of appetite, vomiting, and may even experience seizures . Severe cases often lead to blindness, malnutrition, intellectual disability , and are generally difficult to care for, with a poor prognosis. However, some children with mild cases can gradually recover with timely treatment.
Hydrocephalus is primarily caused by impaired cerebrospinal fluid circulation. The main causes of this impaired circulation include congenital malformations (aqueductal stenosis, spina bifida , fourth ventricle foramen occlusion, etc.), intracranial hemorrhage due to neonatal hypoxia and birth trauma , adhesions secondary to meningitis, and tumors. Traditional Chinese medicine believes that the causes of hydrocephalus can be summarize as follows: congenital deficiency, kidney qi deficiency, external pathogenic factors causing heat toxins to accumulate and attack the brain, acquired malnutrition, post-illness imbalance, spleen deficiency leading to water retention, or water failing to nourish wood, causing liver yang hyperactivity and upward flow of wind and water, or blood stasis obstructing the meridians, compressing the brain marrow, and blocking the brain orifices, ultimately leading to widened fontanelle and craniotomy.
Children with hydrocephalus typically present with an enlarged head disproportionate to their trunk. An enlarged and bulging anterior fontanelle (sometimes connected to the posterior fontanelle). A protruding forehead, engorged scalp veins , sunken orbital roof due to pressure, downward gaze, and exposure of the upper sclera, forming a “sunset sign.” Percussion of the head produces a cracked pot sound. Diagnosis can be confirm via CT and MRI.
Symptoms and signs of hydrocephalus in children
Compared to adults, the clinical manifestations of hydrocephalus in children vary according to the patient’s age of onset. In acute hydrocephalus in infants, symptoms of increased intracranial pressure are usually obvious, with sutures splitting, a bulging anterior fontanelle, thinning of the scalp, and clearly visible and distended scalp veins. The head may also show translucency when illuminated with a strong light. Percussion of the top of the head in children with hydrocephalus produces a solid tympanic sound, known as the “broken pot sound” or Macewen’s sign. Affected children are easily irritate, exhibit apathy, poor appetite, and persistent, high-pitched, short, abnormal crying.
Both eyes are in a downward gaze position, without ptosis of the upper eyelids; the lower half of the eyeball may appear sunken to the lower eyelid margin, with part of the cornea above the lower eyelid margin. The sclera of the upper eyelid may invert, revealing the white of the eye, also known as the sunset phenomenon. Dissociation occurs when the eyes look upward or downward, along with gaze palsy and nystagmus, which are related to dysfunction of the brainstem nuclei around the aqueduct.
As hydrocephalus progresses, the brainstem shifts downward, and the abducens nerve and other cranial nerves are stretch, leading to oculomotor disturbances . In children under two years old, amblyopia may occur due to abnormal eye movements. Papilledema is not prominent and rare in congenital hydrocephalus , but retinal varicose veins are a reliable sign of hydrocephalus. Motor abnormalities mainly include spastic paralysis of the limbs, primarily the lower limbs. Mild cases present with heel tension and foot drop, while severe cases exhibit a spastic gait, also known as scissor gait, which can sometimes be difficult to distinguish from cerebral palsy.
Due to involvement of the anterior ventricles of the third ventricle and the hypothalamus and infundibulum, various endocrine disorders may occur , such as precocious puberty or delayed puberty, short stature, and other symptoms of decreased hormone levels. Furthermore, syringomyelia with hydrocephalus often presents with lower limb movement disorders, while syringomyelia with spinal cord dysplasia often presents with scoliosis.
How is hydrocephalus diagnosed in children?
In infancy and early childhood, the primary diagnostic sign of hydrocephalus is an abnormally enlarge head, with a head circumference disproportionate to the child’s age. Regularly measuring an infant’s head circumference helps in the early detection of hydrocephalus and allows for a definitive diagnosis before typical signs appear, enabling timely treatment. Typical signs include a large head and small face, drooping eyeballs, and often strabismus. The scalp appears shiny and taut, with distended veins in the forehead, and abnormally progressive enlargement of the fontanelle and sutures. Aside from intellectual developmental delays , these subtle, daily changes may go unnoticed by parents.
Hydrocephalus in children progresses, known as active hydrocephalus, and many infants will die if left untreated. Naturally surviving infants may develop quiescent hydrocephalus, characterized by intellectual disability, various types of spasticity, visual impairment including blindness, and many other abnormalities. In newborns, even with ventricular enlargement or hydrocephalus, the anterior fontanelle may still be sunken, especially in low birth weight infants, whose heads may be smaller than normal due to dehydration. Furthermore, premature infants are prone to intraventricular hemorrhage, often resulting in ventricular enlargement and abnormally large head circumference within 6–14 weeks after the neonatal period; however, this process is self-limiting.
While abnormally large head circumference is an important sign of hydrocephalus, there is no absolute relationship between the two. A thorough understanding of the entire clinical process, including the perinatal period , is necessary for continuous observation of ventricular dilation. Ultrasound is a simple, non-invasive, and reproducible reliable method for observing hydrocephalus patients. Once a diagnosis of progressive hydrocephalus is establish, neuroimaging examinations such as head CT and MRI can be perform to rule out intracranial tumors, congenital malformations , and obstructive cerebrospinal fluid lesions. Water-soluble contrast agents and radionuclide scanning are helpful in the diagnosis of obstructive hydrocephalus , but their use is generally limited.
Differential diagnosis of pediatric hydrocephalus
Hydrocephalus in children needs to be differentiate from the following diseases.
1. Chronic subdural effusion or hematoma often has a history of birth injury. The lesion can be unilateral or bilateral, and papilledema is common. The sunset sign is negative. Aspiration of hemorrhagic or pale yellow fluid from the subdural space via puncture of the anterior fontanelle can confirm the diagnosis. Cerebral angiography, CT, or MRI can also differentiate the condition.
2. Neonatal intracranial tumors: Neonatal intracranial tumors often present with increased head circumference or secondary hydrocephalus . Ventriculography, CT scan, or MRI can confirm the diagnosis.
3. In vitamin D deficiency, the head circumference may increase, resulting in a square skull. The anterior fontanelle may be enlarge with low tension, along with other manifestations of vitamin D deficiency .
4. Congenital macrocephaly has no signs of hydrocephalus, a negative sunset sign, no enlargement of the ventricular system, and no increased intracranial pressure. It can be diagnose by CT scan.
How to treat hydrocephalus in children?
Treatment for hydrocephalus can be divide into conservative and surgical methods. Conservative treatment involves keeping the head elevate, restricting fluid intake, and administering diuretics, but its effectiveness is limited. Surgical treatment offers various options, with ventriculoperitoneal shunt being the most common in China . This involves surgically inserting a silicone tube into the lateral ventricle at one end and into the peritoneum at the other, with the tube embedded subcutaneously and connected by an anti-reflux pump. This allows the high-pressure cerebrospinal fluid in the cranial cavity to flow into the peritoneum.
The peritoneum then absorbs the fluid, relieving intraventricular pressure and promoting brain cell growth and development. Brain tissue development continues rapidly after birth. The brain weighs 350g at birth, 900g at one year old, and the rate of weight gain slows after one year, reaching an adult brain weight of 1.5kg. Therefore, when hydrocephalus is diagnose in a child, surgery should be perform as early as possible. Some patients may experience normal motor and intellectual development after surgery.
