
Osteoporosis ICD 10: The Latest Updates You Need to Know
Healthcare providers face a critical challenge in managing osteoporosis – a condition affecting millions worldwide that weakens bones and increases fracture risks. The October 2023 updates to ICD-10 coding bring significant changes to how we document and track osteoporosis cases.
Why These Updates Matter
- Precise coding ensures accurate patient records
- Improves insurance claim processing
- Enables better tracking of treatment outcomes
- Supports research and population health studies
The latest ICD-10 updates introduce 395 new billable codes, with specific additions for osteoporosis-related conditions. These changes reflect the growing need for detailed documentation in modern healthcare, particularly for complex conditions like osteoporosis.
What You’ll Learn
- New diagnosis codes for osteoporotic fractures
- Updated coding guidelines for 2024
- Specific changes in pelvic fracture documentation
- Essential coding rules for healthcare providers
These updates represent a significant shift in how we document osteoporosis cases. Whether you’re a healthcare provider, medical coder, or administrator, understanding these changes is crucial for maintaining compliance and ensuring proper patient care documentation.
[Stay current with these coding updates to optimize your practice’s efficiency and accuracy in osteoporosis care management.]
Understanding Osteoporosis
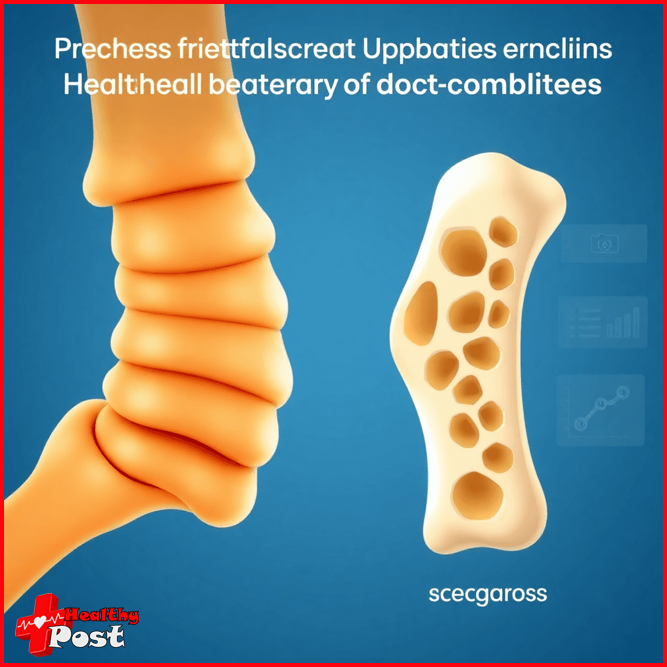
Osteoporosis is a skeletal disorder characterized by compromised bone strength, leading to increased fracture risk. The condition causes bones to become porous, fragile, and susceptible to breaks – even from minor falls or impacts.
Think of healthy bones as a well-constructed honeycomb structure. In osteoporosis, the holes and spaces within this structure grow larger, reducing bone density and strength. This progressive condition often develops silently, earning its nickname “the silent disease.”
Types of Osteoporosis:
- Age-related (Primary Type 1): Develops naturally with aging, typically affecting those over 70
- Postmenopausal (Primary Type 2): Occurs in women after menopause due to decreased estrogen production
- Drug-induced (Secondary): Results from medications like corticosteroids or certain cancer treatments
- Idiopathic: Develops without an identifiable cause, rare but can affect young adults
Bone Density: The Key Diagnostic Tool
Bone density measurement serves as the primary diagnostic tool for osteoporosis. Medical professionals use Dual-energy X-ray Absorptiometry (DXA) scans to:
- Measure bone mineral density (BMD)
- Compare results to standard values
- Generate T-scores indicating bone strength
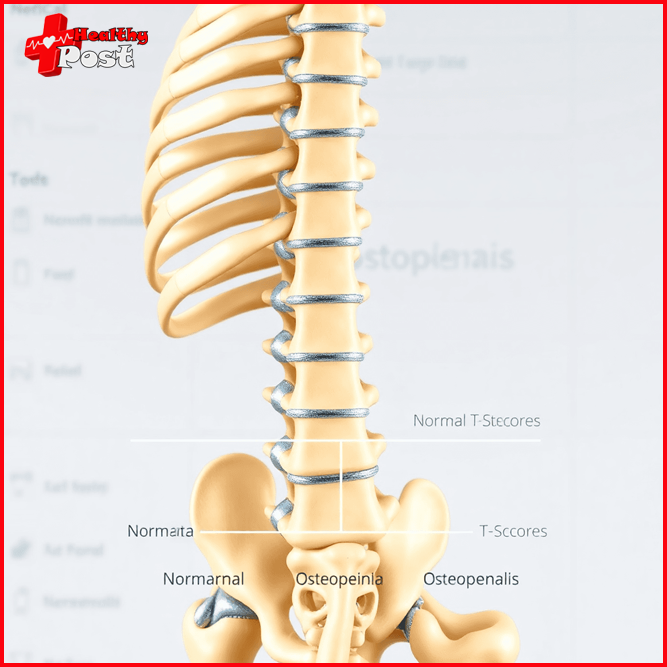
The World Health Organization defines osteoporosis based on these T-scores:
Normal: T-score above -1.0 Osteopenia: T-score between -1.0 and -2.5 Osteoporosis: T-score below -2.5
Regular bone density testing becomes crucial for:
- Women aged 65 and older
- Men aged 70 and older
- People with significant risk factors
- Individuals taking bone-affecting medications
Understanding bone density measurements helps healthcare providers track disease progression and determine appropriate treatment strategies. These measurements also play a vital role in proper medical coding and documentation.
Understanding the ICD-10-CM Coding System
The ICD-10-CM (International Classification of Diseases, 10th Revision, Clinical Modification) is a standardized system used to classify and code health conditions. It provides healthcare providers with a comprehensive set of codes to accurately document diagnoses.
Structure of ICD-10-CM Codes
ICD-10-CM codes are structured in a specific way:
- Category (first three characters): Identifies the general condition
- Etiology (characters 4-6): Specifies the cause or type of condition
- Anatomic Site (character 7): Indicates the affected body part
Relevant Codes for Osteoporosis
When it comes to coding osteoporosis, the “M” series codes are particularly important:
- M80: Osteoporosis with pathological fracture
- M81: Osteoporosis without pathological fracture
- M85: Other disorders of bone density and structure
Importance of Accurate Coding
Accurate coding practices have a direct impact on various aspects of healthcare:
- Patient Care: Proper documentation ensures that appropriate treatment protocols are followed.
- Research: Reliable data collection for medical studies is dependent on accurate coding.
- Reimbursement: Correct billing and insurance claims processing rely on precise coding.
- Healthcare Analytics: Tracking disease patterns and treatment outcomes requires accurate coding.
Regular Updates to the ICD-10-CM System
The ICD-10-CM system needs regular updates to keep up with new medical discoveries and changing healthcare needs. Healthcare providers must stay informed about these updates to maintain coding accuracy.
Benefits of Specificity in Coding
The specificity of the ICD-10-CM system allows for detailed tracking of osteoporosis cases. This includes information such as:
- Disease progression
- Fracture locations
- Associated conditions
- Treatment responses
This level of detail supports better coordination of patient care and helps healthcare facilities comply with regulatory requirements.

Latest Updates in ICD-10-CM for Osteoporosis
The 2024 ICD-10-CM code updates bring significant changes to osteoporosis coding, effective October 1, 2023. These updates introduce eight new billable diagnosis codes, designed to provide enhanced specificity for healthcare providers documenting osteoporosis-related fractures.
New M80.0B Series Codes for Age-Related Osteoporosis
The M80.0B series focuses on age-related osteoporosis with current pathological fractures:
- M80.0B – Age-related osteoporosis with current pathological fracture, pelvis
- M80.0B1 – Age-related osteoporosis with current pathological fracture, right pelvis
- M80.0B2 – Age-related osteoporosis with current pathological fracture, left pelvis
- M80.0B9 – Age-related osteoporosis with current pathological fracture, unspecified pelvis
New M80.8B Series Codes for Other Types of Osteoporosis
The M80.8B series addresses other types of osteoporosis with current pathological fractures:
- M80.8B – Other osteoporosis with current pathological fracture, pelvis
- M80.8B1 – Other osteoporosis with current pathological fracture, right pelvis
- M80.8B2 – Other osteoporosis with current pathological fracture, left pelvis
- M80.8B9 – Other osteoporosis with current pathological fracture, unspecified pelvis
These new codes represent a significant advancement in medical coding precision. Prior to this update, healthcare providers had to code pelvic fractures under femur fractures, leading to potential inaccuracies in documentation and billing.
Key Benefits of the New Codes
The updated coding system offers several advantages:
- Anatomical Precision – Clear distinction between right, left, and unspecified pelvic fractures
- Diagnostic Accuracy – Separate codes for age-related and other types of osteoporosis
Purpose and Benefits of New Codes
The 2024 ICD-10-CM updates bring significant improvements to osteoporosis coding accuracy. These changes address a critical gap in the previous coding system where pelvic fractures were incorrectly categorized under femur fractures.
1. Enhanced Anatomical Precision
- Distinct identification of right, left, and unspecified pelvic fractures
- Clear differentiation between age-related and other types of osteoporosis
- Specific anatomical location tracking for better patient care monitoring
2. Improved Documentation Benefits
- Detailed medical records for comprehensive patient history
- Better tracking of fracture patterns and treatment outcomes
- Streamlined communication between healthcare providers
3. Reimbursement Advantages
- Accurate billing codes reduce claim denials
- Proper documentation supports medical necessity
- Specific coding allows appropriate payment rates
4. Healthcare Data Analysis
- Better statistical tracking of osteoporosis-related fractures
- Enhanced ability to study treatment effectiveness
- Improved population health management capabilities
5. Clinical Research Impact
- More precise data collection for osteoporosis studies
- Better understanding of fracture patterns and risk factors
- Enhanced ability to track treatment outcomes
6. Quality Reporting Benefits
- Accurate measurement of care quality metrics
- Better compliance with reporting requirements
- Enhanced ability to track patient outcomes
These new codes represent a significant step forward in healthcare documentation. Healthcare providers can now capture specific details about osteoporotic fractures with unprecedented accuracy. This granular level of detail supports both immediate patient care needs and broader healthcare system goals.
The updated coding system also aids in risk management and treatment planning. By accurately documenting fracture locations and types, healthcare providers can develop more targeted treatment strategies and better predict potential complications.
Risk Factors for Osteoporosis
Understanding risk factors plays a vital role in osteoporosis prevention and management. Medical professionals use these risk factors alongside ICD-10 codes to create comprehensive patient profiles and treatment plans.
Uncontrollable Risk Factors
- Age: Bone density naturally decreases after age 50
- Gender: Women face higher risks, particularly post-menopause
- Family history of osteoporosis
- Small, thin body frame
- Certain ethnicities (Asian and Caucasian populations show higher risk)
Lifestyle-Related Risk Factors
- Smoking – reduces bone mass
- Excessive alcohol consumption
- Sedentary lifestyle
- Poor nutrition, especially low calcium intake
- Vitamin D deficiency
Medical Conditions and Medications
- Rheumatoid arthritis
- Type 1 diabetes
- Liver or kidney disease
- Long-term use of:
- Corticosteroids
- Anti-seizure medications
- Proton pump inhibitors
Women experience a dramatic increase in osteoporosis risk during menopause due to decreased estrogen production. Men typically develop osteoporosis 10 years later than women, but their risk steadily increases with age. Healthcare providers use these risk factors to determine appropriate screening schedules and preventive measures, documenting findings with specific ICD-10 codes for precise medical records.
Bone Health Testing and Diagnosis
Regular bone health testing plays a vital role in early detection and management of osteoporosis. A bone density test provides crucial insights into bone strength and potential fracture risks.
Primary Testing Methods:
- DXA (Dual-energy X-ray Absorptiometry): The gold standard for bone density measurement, this painless, non-invasive procedure takes 10-30 minutes to complete and measures specific areas such as the hip, spine, and wrist.
- Quantitative CT Scan: This method creates detailed 3D images of bones and is useful for people unable to undergo DXA. It also provides separate measurements for different bone types.
- Bone Marker Tests: These blood and urine tests measure bone formation and breakdown rates, helping to monitor treatment effectiveness.
When to Get Tested:
- Women age 65 and older
- Men age 70 and older
- People with significant height loss
- Those taking medications affecting bone density
- Individuals with specific medical conditions
Test results use T-scores to indicate bone density levels:
- Normal: -1 and above
- Osteopenia: between -1 and -2.5
- Osteoporosis: -2.5 or lower
Healthcare providers use these results alongside medical history and risk factors to develop personalized treatment strategies and monitoring plans.
Treatment Options for Osteoporosis
Managing osteoporosis requires a comprehensive treatment approach combining medical interventions with lifestyle modifications. Here’s what you need to know about available treatment options:
Medications
- Bisphosphonates: Alendronate, Risedronate, Ibandronate
- Slow down bone loss
- Reduce fracture risk
- Available in oral and injectable forms
- Hormone-Related TherapyEstrogen therapy for postmenopausal women
- Selective Estrogen Receptor Modulators (SERMs)
- Calcitonin for pain management
- Biological AgentsDenosumab – targets bone breakdown
- Teriparatide – stimulates new bone formation
Lifestyle Modifications
- Exercise ProgramWeight-bearing activities
- Resistance training
- Balance exercises to prevent falls
- Dietary ChangesCalcium-rich foods
- Vitamin D supplementation
- Reduced alcohol consumption
- Smoking cessation
Alternative Therapies
- Acupuncture for pain management
- Physical therapy
- Occupational therapy for daily activities
Your healthcare provider will create a personalized treatment plan based on factors like age, gender, fracture risk, and overall health status. Regular monitoring helps adjust treatments as needed for optimal bone health maintenance.
Understanding Coding Rules and Guidelines
Accurate coding for osteoporosis requires attention to specific guidelines and documentation requirements. Here are the essential rules healthcare providers need to follow:
Primary Documentation Requirements:
- Clear identification of osteoporosis type (age-related, post-menopausal, or drug-induced)
- Detailed description of any associated fractures
- Specific anatomical location affected
- Laterality information when applicable
Key Coding Principles:
- Use M80 codes for osteoporosis with current pathological fracture
- Apply M81 codes for osteoporosis without current pathological fracture
- Include 7th character extensions when required:
- A: initial encounter
- D: subsequent encounter
- G: healing
- S: sequela
Documentation Best Practices:
- Record bone density T-scores
- Note relevant risk factors
- Document current medications
- Include treatment history
Common Coding Mistakes to Avoid:
- Missing laterality specifications
- Incorrect sequencing of codes
- Overlooking pathological fracture documentation
- Using unspecified codes when more specific options exist
The 2024 updates introduce new specificity requirements for pelvic fractures, separating them from femoral fractures. These changes demand careful attention to anatomical details and proper code selection based on precise documentation.
Conclusion
Staying current with ICD-10 coding updates for osteoporosis is essential for healthcare providers and coding professionals. The latest updates, including the M81.0 diagnosis code details and new pelvic fracture codes, reflect the evolving nature of medical coding standards.
We recommend:
- Bookmarking the CMS website for quick access to coding updates
- Joining professional coding organizations for continuous learning
- Participating in regular training sessions on new coding guidelines
- Creating a network of coding professionals to share knowledge and insights
The field of medical coding continues to grow more precise, offering better ways to document patient care and streamline billing processes. Your commitment to understanding these changes directly impacts patient care quality and healthcare facility operations.
Take time to review the resources shared in this guide, particularly the new M80.0B series codes for osteoporosis with pathological fractures. Your dedication to accurate coding helps build a more efficient healthcare system for everyone involved.
FAQs (Frequently Asked Questions)
What is osteoporosis and why is it significant?
Osteoporosis is a medical condition characterized by weakened bones and reduced bone density, making individuals more susceptible to fractures. Its significance lies in the impact it has on health, particularly in older adults, where it can lead to severe complications from fractures.
What are the types of osteoporosis?
The primary types of osteoporosis include age-related osteoporosis, postmenopausal osteoporosis, drug-induced osteoporosis, and idiopathic osteoporosis. Each type has different causes and risk factors associated with it.
What are the latest updates in the ICD-10-CM coding for osteoporosis?
The latest updates as of October 1, 2023, include new diagnosis codes specifically for osteoporosis with pathological fractures, particularly within the M80.0B series. These changes aim to enhance accuracy in coding and improve patient record clarity.
Why is accurate coding important in healthcare for osteoporosis?
Accurate coding for osteoporosis is crucial as it affects patient care, reimbursement processes, and statistical data collection. It ensures that patients receive appropriate treatment and that healthcare providers are compensated fairly for their services.
What are common risk factors for developing osteoporosis?
Common risk factors for osteoporosis include advanced age, gender (with women being at higher risk), family history of the disease, low body weight, certain medications, and lifestyle factors such as smoking and excessive alcohol consumption.
What treatment options are available for osteoporosis?
Treatment options for osteoporosis typically include medications that strengthen bones (such as bisphosphonates), hormone replacement therapy, dietary supplements like calcium and vitamin D, and lifestyle changes such as regular exercise to improve bone health.

2 thoughts on “Osteoporosis ICD 10: The Latest Updates You Need to Know”