
7 Essential Diazepam Injection Facts for Safer Use
When you or someone you love receives a Diazepam Injection, it can feel worrying and confusing. Understanding why it is used, how it works, and what to watch for can make the experience much safer and less frightening. ❤️
This guide walks you through seven key facts, explained in clear language. It is for patients, caregivers, and anyone who wants to feel more informed before or after treatment.
This article is for education only and not a substitute for medical advice. Always follow your doctor’s instructions.
1. What a Diazepam Injection Is and When It’s Used
Diazepam belongs to a group of medicines called benzodiazepines. These medicines calm overactive brain activity.
The injection form is usually given in hospitals or emergency settings. It is not a routine “at home” medicine.
Doctors use it for situations such as:
- Seizures, including status epilepticus
- Severe muscle spasms
- Serious agitation, often linked to alcohol withdrawal
- Pre‑procedure sedation in some cases
You will usually receive it from:
- An emergency doctor
- An anesthetist
- A nurse or paramedic trained in emergency care
Most people receive this medicine only short term. Long‑term use by injection is rare and usually avoided.
If you are worried about why it has been chosen, ask:
- “Why this medicine and not something else?”
- “What is the goal of this treatment for me?”
Healthcare teams expect and welcome these questions. ✅
2. How It Works in Your Body 🧠
Diazepam boosts the effect of a calming brain chemical called GABA. Think of GABA as a “brake” for overactive brain signals.
When the medicine is injected, it:
- Slows down abnormal electrical activity in the brain
- Relaxes muscles
- Reduces anxiety and agitation
- Can cause drowsiness or sleep
How quickly it acts depends on how it is given.
- In a vein (IV), it works within minutes.
- In a muscle (IM), it can be slower and less predictable.
Its calming effect can last for several hours. However, it also lingers in the body longer, which is why drowsiness may continue.
Your liver breaks down the medicine, and your kidneys clear it. People with liver or kidney disease may need extra monitoring.
If you feel unusually sleepy or confused afterward, let staff know. ⚠️

3. Understanding Diazepam Injection side effect risks ⚠️
Like every strong medicine, there is a risk of unwanted effects. Knowing the most important Diazepam Injection side effect patterns can help you speak up early.
Common, usually short‑term effects include:
- Drowsiness or feeling very sleepy
- Dizziness or light‑headedness
- Muscle weakness
- Confusion, especially in older adults
- Blurred vision
Less common but serious effects include:
- Breathing that becomes slow or shallow
- Very low blood pressure
- Severe allergic reaction
- Paradoxical reactions, like agitation or aggression instead of calm
In older people, those with lung disease, or those using opioids, breathing problems are a key worry. Staff often monitor:
- Breathing rate
- Oxygen levels
- Blood pressure
For more detail on Diazepam Injection side effect profiles and safety information, you can review the trusted summary from Diazepam Injection side effect.
Warning signs to report immediately
Tell a doctor or nurse at once if you notice:
- Trouble breathing or feeling like you cannot catch your breath
- Chest pain or a racing heart
- Swelling of face, lips, tongue, or throat
- Sudden severe confusion or strange behavior
Family members can help by watching for change. Sometimes the person who received the medicine cannot notice changes clearly.
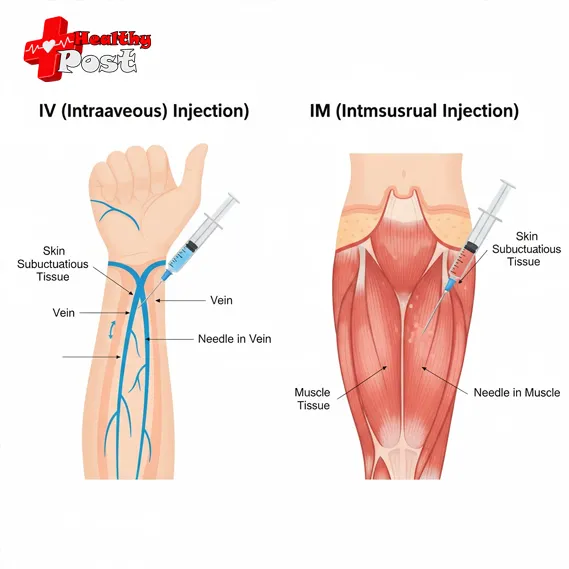
4. diazepam injection iv or im: how professionals decide
The medicine can be given into a vein (IV) or a muscle (IM). The choice is not random. It depends on urgency, setting, and your condition. 💉
IV (intravenous) injection
IV means the medicine goes straight into a vein.
Advantages:
- Works very fast
- Dose can be adjusted more accurately
- Easier to control in a monitored setting
Disadvantages:
- Needs IV access and trained staff
- Higher risk if given too fast
- Requires close monitoring of breathing and blood pressure
IM (intramuscular) injection
IM means it goes into a large muscle, often the thigh or buttock.
Advantages:
- Useful when IV access is difficult
- Can be given quickly in the field (for example, by paramedics)
Disadvantages:
- Slower and more variable absorption
- Can be painful at the injection site
- Less ideal in emergency seizures when rapid effect is needed
Healthcare teams follow guidelines on diazepam injection iv or im for safer use. You can read more professional guidance in the monograph at diazepam injection iv or im.
Quick comparison table
| Route | Typical Use Case | Onset of Effect | Monitoring Needs | Key Caution |
|---|---|---|---|---|
| IV (intravenous) | Emergency seizures, ICU, theater | Minutes | Close heart and breathing checks | Must be given slowly by trained staff |
| IM (intramuscular) | When IV access is not possible or delayed | Slower, variable | Standard observation | Less predictable effect |
You can ask your doctor:
- “Why did you choose IV instead of IM for me?”
- “How long should I expect the effect to last?”
Clear answers can increase trust and reduce fear. 😊
5. What to Expect Before, During, and After the Injection
Knowing what usually happens can make the process less stressful.
Before the injection
Staff will usually:
- Check your identity
- Review allergies and current medicines
- Measure blood pressure, pulse, and oxygen level
- Explain why the medicine is needed, if time allows
Before a nurse gives a Diazepam Injection, they confirm the right dose and route. They also ensure emergency equipment is nearby, especially in an emergency room or intensive care unit.
If you are conscious and able, share:
- Past reactions to benzodiazepines
- Lung or heart disease
- Regular use of opioids, alcohol, or sleep medicines
This information helps staff keep you safer.
During the injection
You may notice:
- A cool feeling in the vein, if IV
- Brief discomfort in the muscle, if IM
- Drowsiness starting fairly quickly
Staff will keep an eye on:
- Your breathing pattern
- Skin color and comfort
- Blood pressure and heart rate in higher‑risk cases
If anything feels wrong, say so, even if you think it is “small.”
After the injection
It is normal to feel:
- Sleepy or tired
- Less anxious
- A bit unsteady when walking
You may need someone to:
- Help you walk safely
- Stay with you until you are fully alert
- Make sure you do not drive or operate machines
Ask before you leave:
- “When is it safe for me to drive again?”
- “What symptoms should make me return to the hospital?”
6. Who Should Be Extra Careful ⚠️
Some people are more sensitive to this medicine. Extra care and monitoring may be needed in these groups:
Older adults
Older adults often feel stronger and longer‑lasting effects.
Risks include:
- Falls due to dizziness or weakness
- Delirium or sudden confusion
- Worsening memory problems
Lower doses and closer monitoring are common in this group.
People with breathing problems
Conditions such as:
- COPD
- Severe asthma
- Sleep apnea
can make sedating medicines riskier. Diazepam can slow breathing further, especially when combined with:
- Opioid painkillers
- Alcohol
- Other sedatives
People with liver or kidney disease
These organs clear the medicine from the body. When they do not work well, diazepam can build up and cause:
- Excessive drowsiness
- Prolonged confusion
People with a history of substance use disorder
Benzodiazepines can be habit‑forming. While emergency use is sometimes necessary, doctors try to:
- Avoid repeated doses without a clear plan
- Use the lowest effective dose
- Combine with non‑drug strategies where possible
If you have such a history, tell your team openly. It helps them protect you, not judge you.
7. How to Use This Treatment as Safely as Possible ✅
You may not control when an emergency injection is given. Yet you can still play an active role in safety.
Share your full medical story
When possible, tell staff about:
- All prescription medicines
- Over‑the‑counter drugs and herbal products
- Alcohol use and recreational drugs
This can prevent dangerous combinations.
Ask key safety questions
If there is time before the injection, you can ask:
- “What are the main benefits for me right now?”
- “What side effects should we watch for?”
- “How long will I be observed afterward?”
After the injection, ask:
- “What should I avoid for the next 24 hours?”
These questions are not confrontational. They are part of good, shared decision‑making.
Follow recovery advice carefully
Common instructions include:
- Do not drive for at least 24 hours, or as told
- Avoid alcohol and sedative medicines unless your doctor agrees
- Have someone stay with you if you feel weak or unsteady
If you go home after treatment, consider planning:
- A responsible adult to accompany you
- Rest time with no major tasks
- A list of emergency numbers in case symptoms worsen
Learn about non‑drug support
For seizures, muscle spasms, or severe anxiety, treatment often works best when:
- Medicines
- Lifestyle measures
- Psychological support
are combined. You might benefit from:
- Counseling or therapy
- Sleep hygiene and stress management
- Support groups for epilepsy, anxiety, or alcohol withdrawal
Ask your team about long‑term plans beyond the emergency visit. This can reduce the need for repeated injections in the future. 🌱
Frequently Asked Questions (FAQs)
1. Can I receive this injection at home?
Usually no. This medicine is normally given in hospitals, clinics, or by emergency services. At‑home use would be rare and only under strict medical supervision.
2. Is it safe to drink alcohol after the injection?
No. Alcohol adds to the sedative effect and can slow breathing. Avoid alcohol until your doctor confirms it is safe to drink again.
3. How long will I feel drowsy?
Many people feel drowsy for several hours. Some feel “off” until the next day. The exact time depends on your dose, age, liver health, and other medicines.
4. Can this injection be addictive?
A single emergency dose is unlikely to cause addiction. But frequent or repeated doses can contribute to dependence, especially in people with past substance use concerns.
5. What should family members watch for after discharge?
Family should watch for:
- Troubled or slow breathing
- Struggling to stay awake
- Sudden confusion or strange behavior
- Chest pain or severe dizziness
If any of these appear, seek urgent medical help.
6. Is it safe during pregnancy?
Use in pregnancy is a complex decision. In emergencies, doctors may still use it if the benefits outweigh risks. Pregnant patients should discuss this with their obstetric and medical teams whenever possible.
Final Thoughts on Safer Use of Diazepam Injection 💬
Used carefully, a Diazepam Injection can be an important short‑term tool in serious situations. It can stop seizures, calm dangerous agitation, and ease severe muscle spasms.
The key to safer use is:
- Clear communication with healthcare professionals
- Honest sharing of your medical history
- Careful monitoring for side effects
- Respecting safety advice after treatment
You are allowed to ask questions, express fears, and request explanations. Being informed does not mean refusing treatment. It means partnering with your medical team so that treatment is as safe and effective as possible.
If you have ongoing worries, book time with your doctor to review what happened, why this medicine was used, and how future emergencies will be handled. Feeling prepared can greatly reduce fear if it is ever needed again. ❤️

