7 Critical Signs to Know Before Taking the Achilles Tendon Rupture Test
Knowing the signs of an Achilles tendon rupture can save you from severe complications. This injury strikes during common activities like sports or even daily movements.
The Achilles tendon rupture test helps confirm if you’ve damaged this vital tissue. Understanding the warning signs before taking this test is crucial for your health.
Think of your Achilles tendon as a strong rubber band connecting your heel to your calf muscles. When it snaps, you’ll need quick medical help to prevent long-term problems.
We’ll explore 7 critical signs that suggest you might need an Achilles tendon rupture test:
- Sharp pain sensations
- Visible swelling patterns
- Walking difficulties
- Physical changes
- Movement limitations
- Medical test results
- Risk factors to consider
These signs will help you make informed decisions about seeking medical care. Let’s dive into each sign to understand what your body might be telling you.
Key Signs and Symptoms of Achilles Tendon Rupture
The Achilles tendon rupture test helps identify damage in this vital tendon. Recognizing these signs can lead to faster diagnosis and better recovery outcomes.
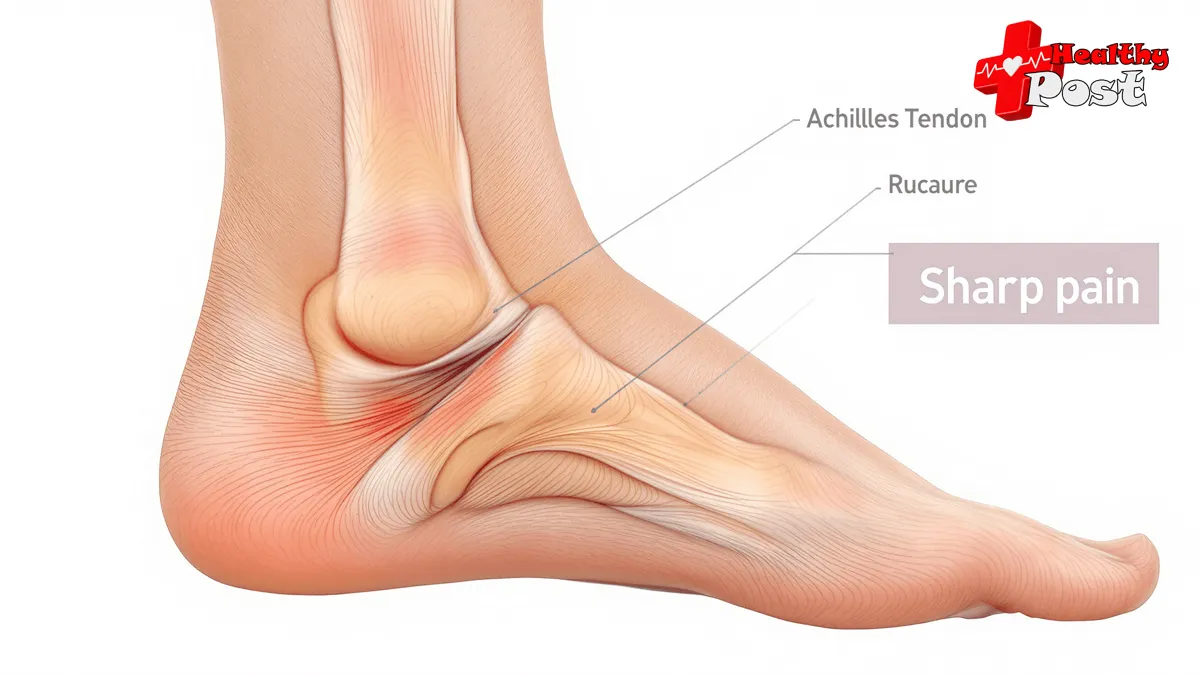
1. Sudden Sharp Pain and Popping Sensation at the Back of the Ankle
A sudden sharp pain strikes the back of your ankle during the injury. This pain feels like someone hit your heel with a stick. Many people hear a loud “pop” or snap when the tendon breaks.
The pain intensity ranges from mild to severe, depending on:
- Complete tear of the tendon
- Partial tear
- Location of the rupture
- Individual pain tolerance
Common activities that trigger rupture:
- Running and stopping quickly
- Starting a sprint
- Landing from a jump
- Missing a step while walking
- Falling from a height
The popping sound happens when the tendon fibers snap apart. This sound might be loud enough for others nearby to hear it too.
Key pain characteristics:
- Starts without warning
- Feels like a direct hit to the heel
- Can make you fall or stumble
- May fade to a dull ache
- Gets worse with movement
Many patients describe the sensation as:
“It felt like someone kicked me hard in the back of my ankle”
The location of pain sits about 2-6 centimeters above the heel bone. This spot marks where the Achilles tendon typically breaks.
Physical changes after the pop:
- Immediate weakness in the affected foot
- Trouble standing on tiptoes
- Pain when trying to point toes down
- Difficulty pushing off while walking
The combination of sudden pain and popping marks the start of other symptoms. These signs help doctors determine if you need an Achilles tendon rupture test.
2. Swelling and Bruising in the Heel Area
A ruptured Achilles tendon causes blood vessels to break near the injury site. This creates visible signs within hours:
- Dark purple bruising spreads across the back of the heel
- Noticeable swelling extends from the heel up to the calf
- The affected area feels warm and tender to touch
- Skin around the heel might appear shiny or stretched
The size of bruising varies between patients:
- Mild cases: Light bruising limited to heel area
- Severe cases: Extensive bruising reaching up to mid-calf
Your doctor will check these visual markers during examination:
- Compare both ankles side-by-side
- Measure swelling circumference
- Document bruising patterns
- Test skin temperature differences
A quick self-check involves gently pressing the swollen area. If pressing leaves a temporary dent (pitting edema), seek medical attention right away.
The combination of swelling and bruising often peaks 2-3 days after injury. These visible signs help healthcare providers assess injury severity and plan appropriate treatment.
3. Difficulty Walking and Weakness in the Affected Leg
A ruptured Achilles tendon makes simple walking tasks feel impossible. You might notice:
- Inability to climb stairs
- Struggling to stand on tiptoes
- Problems pushing off while walking
- Difficulty maintaining balance
The affected leg feels weak and unstable, like it can’t support your body weight. Many people describe it as walking through quicksand or having a “dead” foot.
Daily activities become challenging:
- Getting out of bed
- Walking to the bathroom
- Standing up from a chair
- Moving around the house
The weakness stems from the disconnection between your calf muscle and heel bone. Your brain sends signals to move your foot, but the broken tendon can’t transmit these commands.
Common Signs of Walking Difficulty:
- Limping
- Dragging the affected foot
- Compensating with the other leg
- Taking smaller steps
- Avoiding weight on the injured foot
This combination of weakness and walking problems often forces people to use crutches or other walking aids for support.
4. Visible Swelling or Gap Above the Heel Where the Tendon is Ruptured
One of the most obvious signs of an Achilles tendon rupture is a noticeable gap or indentation above your heel. This gap is where the tendon has torn, creating a visible dip in the normal shape of your leg.
What to Look For
The gap might look like:
- A deep depression you can feel with your fingers
- A visible dent in the back of your ankle
- An unusual bulge or swelling near the tear
The location of this gap sits about 2-6 centimeters above your heel bone. You might notice this gap becomes more obvious when you:
- Stand on your tiptoes
- Flex your foot downward
- Compare it to your uninjured leg
Signs of Inflammation
The area around the gap often shows signs of:
- Soft tissue swelling
- Skin discoloration
- Tenderness to touch
- Changed skin temperature
How to Check for a Rupture
A quick self-check involves gently running your fingers along the back of your ankle. A healthy Achilles tendon feels like a firm, continuous cord. A ruptured tendon will have a distinct interruption in this smooth surface.
5. Difficulty Performing Plantar Flexion (Pointing Foot Downward) with the Affected Leg
A key sign of Achilles tendon rupture is the inability to point your foot downward. This movement, called plantar flexion, becomes challenging due to the damaged tendon.
Here’s what you might notice:
- Your foot feels weak when trying to push down
- Standing on tiptoes becomes impossible
- Basic activities like climbing stairs feel unstable
- Pushing off while walking creates discomfort
A simple test you can try at home:
- Sit with your legs straight
- Try to point your toes toward the floor
- Compare the movement with your unaffected foot
Warning Signs During Movement:
- Limited range of motion
- Weakness in the affected foot
- Sharp pain during attempted movement
- Inability to generate force
The Achilles tendon plays a vital role in plantar flexion. When damaged, this basic foot movement becomes restricted. Your healthcare provider will assess this limitation during examination to determine the extent of injury.
Many patients describe feeling disconnected from their foot during these movements, as if the normal mind-body connection is broken.
6. Positive Thompson Test Result During Physical Examination by a Healthcare Professional
The Thompson test is a crucial diagnostic tool for Achilles tendon rupture. A healthcare provider performs this test by:
- Having the patient lie face down
- Keeping the knee bent at 90 degrees
- Squeezing the calf muscle
A healthy Achilles tendon causes the foot to point downward during the squeeze. The absence of this movement signals a possible rupture.
The test’s accuracy rate reaches up to 96% in detecting complete ruptures. Your doctor might notice:
- No foot movement upon calf squeeze
- A visible gap in the tendon area
- Reduced resistance in the affected foot
“The Thompson test provides quick, reliable results without causing additional pain or discomfort to the patient” – American Journal of Sports Medicine
This physical examination helps doctors determine the next steps in treatment. Many healthcare providers combine the Thompson test with imaging studies like MRI or ultrasound for a complete diagnosis.
Risk Factors That Increase Likelihood of Experiencing an Achilles Tendon Rupture
Understanding the risk factors helps identify who needs the 7 Critical Signs to Know Before Taking the Achilles Tendon Rupture Test. These factors play a key role in prevention and early detection.
Key Risk Factors:
- Age (30-40 years)
- Gender differences
- Sports activities
- Medical conditions
- Previous injuries
- Lifestyle choices
1. Age Range Between 30-40 Years Old Being More Prone To Ruptures
The 30-40 age group faces a higher risk of Achilles tendon ruptures. This age range sees peak physical activity mixed with natural tendon changes.
Why this age group?
- Natural tendon degeneration starts
- Active lifestyle maintenance
- Irregular exercise patterns
- Work-life balance stress on body
- Decreased tissue elasticity
A study shows 75% of Achilles tendon ruptures happen to people aged 30-40 during recreational sports. These numbers highlight the need for extra care during physical activities.
Risk Reduction Tips for 30-40 Age Group:
- Regular stretching routines
- Proper warm-up before exercise
- Gradual intensity increases
- Rest between activities
- Quality footwear use
The combination of peak physical activity and beginning tissue changes creates a perfect storm for tendon injuries. People in this age group need regular check-ups and proper exercise guidance.
Research from Sports Medicine Journal shows weekend warriors in this age group face 3x higher rupture risks than regular exercisers.
| Age Group Risk Level Common Activities 30-35 | High | Basketball, Tennis |
| 35-40 | Highest | Running, Soccer |
| 40+ | Moderate | Walking, Swimming |
2. Male Gender Having A Higher Risk Of Experiencing An Achilles Tendon Rupture Than Female Gender
Research shows men face up to 5 times higher risk of Achilles tendon ruptures compared to women. This gender difference stems from several key factors:
- Men tend to participate more in high-impact sports activities
- Male hormones affect tendon structure and healing
- Higher muscle mass puts increased stress on tendons
The risk becomes particularly notable when combined with:
- Age (30-40 years)
- Irregular exercise patterns
- Lack of proper warm-up routines
A study by the American Journal of Sports Medicine found that male recreational athletes aged 30-40 have the highest rupture rates. These statistics highlight why men need extra caution during:
- Weekend sports activities
- Sudden returns to exercise
- High-intensity workouts
- Quick direction changes in sports
Men who experience any concerning symptoms should seek immediate medical attention. Early detection through proper testing helps prevent complete ruptures and ensures better recovery outcomes.
3. Engaging In High-Impact Sports Activities Such As Basketball Or Soccer Increasing The Chances Of Sustaining A Ruptured Achilles Tendon Injury
High-impact sports put intense stress on the Achilles tendon through:
- Quick Direction Changes: Basketball and soccer demand sudden stops and turns
- Jumping Activities: Volleyball and basketball require repeated jumping motions
- Sprint Movements: Track events and soccer involve explosive running bursts
The risk rises when players aged 30-40 return to sports without proper warm-up. A study shows 70% of Achilles ruptures happen during recreational sports activities.
Common high-risk sports include:
- 🏀 Basketball
- ⚽ Soccer
- 🎾 Tennis
- 🏃♂️ Track and field
- 🏐 Volleyball
Athletes should pay attention to early warning signs like heel pain or stiffness during these activities.
Regular stretching and proper footwear can help reduce injury risk. Taking rest days between intense sports sessions allows the tendon to recover.
4. Previous History of Tendon Issues
If you’ve had problems with your tendons in the past, you’re more likely to experience an Achilles tendon rupture. This means that if you’ve had issues with your tendons before, you need to be extra careful and take special precautions before engaging in any intense activities.
Key points about tendinopathy history:
- Damaged tendons heal slower than healthy ones
- Scar tissue makes tendons less flexible
- Weak spots from old injuries can break under stress
- Pain signals often appear before a full rupture
Warning Signs of Tendinopathy:
Morning heel stiffness
Pain during exercise
Tenderness when touching the area
Reduced strength in the affected leg
Proper rehabilitation includes:
- Gradual return to activity
- Specific stretching exercises
- Regular strength training
- Professional medical guidance
The risk doubles for people aged 30-40 with past tendon issues. A physical therapist can create a safe exercise plan to prevent future injuries.
Tendinopathy patients should watch for new pain or weakness. These symptoms need quick medical attention to avoid serious complications.
5. Medication-Related Risks for Achilles Tendon Problems
Some medications can weaken your Achilles tendon structure. Two main types stand out:
1. Corticosteroids
Long-term use of corticosteroids can have detrimental effects on your Achilles tendon, including:
- Damaging tendon tissue
- Reducing collagen production
- Making tendons brittle
- Slowing down the natural healing process
2. Fluoroquinolone Antibiotics
Fluoroquinolone antibiotics, such as Cipro and Levaquin, have been associated with an increased risk of tendon problems, particularly in individuals over 60 years old. These medications can cause inflammation of the tendons, and the effects may persist for weeks even after discontinuing the drug.
Important Warning Signs During Medication Use:
- Ankle stiffness
- Heel pain
- Reduced flexibility
- Unusual sensations in the tendons
The risk of tendon damage rises when combining these medications with:
- High-impact exercises
- Sudden changes in movement patterns
- Heavy lifting activities
- Prolonged physical activity
A study conducted by the FDA indicates that these medications increase the risk of tendon rupture by 4.1 times. Patients taking these drugs should:
- Inform their doctors about any sports activities they engage in
- Be vigilant for early warning signs of tendon problems
- Avoid sudden intense movements that could strain the tendons
- Discuss alternative medication options with their healthcare provider
Your doctor may recommend different treatment approaches if you are actively involved in sports. Regular monitoring and check-ups can help identify early signs of tendon issues and prevent further complications.
6. Health Conditions That Increase Rupture Risk
Extra body weight puts significant stress on the Achilles tendon. People with obesity face a higher chance of tendon damage during daily activities.
Key Health Factors:
- Obesity ImpactAdded pressure on ankle joints
- Reduced blood flow to tendons
- Slower healing process
- Diabetes EffectsWeakened blood vessels
- Nerve damage risks
- Poor tissue repair ability
- Inflammatory ArthritisJoint inflammation
- Tendon weakness
- Reduced flexibility
These health conditions create a perfect storm for tendon problems. The combination often leads to chronic tendon stress and potential rupture.
Regular medical check-ups help track these conditions. A doctor can spot early warning signs of tendon weakness.
Proper weight management reduces tendon strain. Blood sugar control helps protect tendon health in diabetic patients.
Anti-inflammatory treatments benefit arthritis patients. These medications help preserve tendon strength and flexibility.
Early intervention prevents serious complications. Patients with these conditions need extra care during physical activities.
A balanced exercise program strengthens tendons safely. Working with healthcare providers creates effective management strategies.
Diagnosis And Treatment Options For Achilles Tendon Ruptures
A doctor will check the 7 Critical Signs to Know Before Taking the Achilles Tendon Rupture Test during your visit.
Initial Diagnosis Methods:
- Physical examination of the affected area
- Thompson test to check tendon function
- Medical history review
- Discussion of symptoms and injury circumstances
Advanced Diagnostic Tools:
- Ultrasound scanning for real-time tendon viewing
- MRI scans to assess damage extent
- X-rays to rule out other ankle injuries
Treatment Options:
- Non-Surgical TreatmentProtective boot or cast
- Gradual rehabilitation exercises
- Physical therapy sessions
- Regular progress monitoring
- Surgical TreatmentMinimally invasive surgery
- Traditional open surgery
- Post-surgery rehabilitation plan
- Regular follow-up care
Recovery Timeline:
- Non-surgical: 4-6 months
- Surgical: 6-12 months
- Return to sports: 9-12 months
Quick Tip: Early diagnosis leads to better treatment outcomes. Don’t delay seeking medical help if you notice these signs.
Your doctor will create a personalized treatment plan based on factors like age, activity level, and injury severity. Learn more about Achilles tendon injuries from the American Academy of Orthopaedic Surgeons.
FAQs (Frequently Asked Questions)
What are the 7 critical signs to recognize before taking the Achilles tendon rupture test?
The 7 critical signs include sudden sharp pain and popping sensation at the back of the ankle, swelling and bruising in the heel area, difficulty walking and weakness in the affected leg, visible swelling or gap above the heel where the tendon is ruptured, difficulty performing plantar flexion (pointing foot downward) with the affected leg, and a positive Thompson test result during physical examination by a healthcare professional.
Why is early identification of Achilles tendon rupture signs important?
Early identification of Achilles tendon rupture signs is crucial for proper diagnosis and management. Recognizing symptoms like sharp pain, swelling, bruising, and difficulty walking allows timely medical intervention which can improve recovery outcomes and prevent further complications.
Who is at higher risk for experiencing an Achilles tendon rupture?
Individuals aged between 30-40 years old, males, those who engage in high-impact sports such as basketball or soccer, people with a previous history of tendon issues like tendinopathy, users of certain medications such as corticosteroids or fluoroquinolone antibiotics, and individuals with obesity or conditions like diabetes and inflammatory arthritis are at increased risk for Achilles tendon rupture.
What role does the Thompson test play in diagnosing an Achilles tendon rupture?
The Thompson test is a physical examination technique performed by healthcare professionals to confirm an Achilles tendon rupture. A positive result typically indicates a lack of plantar flexion when squeezing the calf muscle, signifying a possible rupture.
How do injuries like swelling or bruising relate to Achilles tendon ruptures?
Swelling and bruising in the heel area are visible indicators that suggest a potential Achilles tendon rupture. These symptoms often accompany sudden sharp pain and difficulty walking, signaling damage to the tendon that requires medical evaluation.
What treatment options are available after confirming an Achilles tendon rupture?
After confirmation through clinical examinations such as ultrasound or MRI scans following the Achilles tendon rupture test, treatment options may include surgical repair or conservative management like immobilization and physical therapy. The choice depends on severity, patient health status, and activity level.

