
5 Shocking Risks of Coronary Stent Surgery You Should Never Ignore
When your doctor suggests coronary stent surgery, it can feel both reassuring and scary. You hope it will prevent a heart attack and let you breathe easier. At the same time, you may wonder what could go wrong. Those worries are natural—and they deserve honest answers. ❤️
This procedure helps many people live longer, more active lives. Still, like any heart intervention, it carries real risks. Some are rare but serious. Others are more common, yet often overlooked. Understanding them does not mean you should refuse treatment. It means you can make informed choices and protect yourself.
In this article, we will walk through five important risks. For each one, you will learn:
- What the risk actually means
- Warning signs to watch for
- How doctors reduce the danger
- What you can do to stay safer
The goal is not to scare you. It is to help you feel informed, prepared, and supported. 💬

1. Risk of Blood Clots Forming Inside the Stent (Stent Thrombosis) ⚠️
One of the most serious risks after stent placement is a clot forming inside the stent. This is called stent thrombosis. It can suddenly block blood flow to the heart muscle. That blockage can trigger a heart attack, even months or years later.
Why clots can form
After the procedure, your artery needs time to heal. The stent is a foreign object. Your blood tends to form clots on foreign surfaces.
To lower this risk, doctors prescribe a combination of blood thinners, often called dual antiplatelet therapy. These medicines make your blood less “sticky.”
Common reasons clots still form include:
- Stopping blood thinner pills too early
- Missing doses often
- Very complex or long stents
- Smoking or uncontrolled diabetes
- Rare reactions to the stent material
Warning signs you should never ignore
Call emergency services right away if you notice symptoms like:
- Sudden chest pain, pressure, or tightness
- Pain spreading to the arm, jaw, back, or neck
- Shortness of breath or trouble catching your breath
- Sweating, nausea, or feeling faint
These signs can appear even long after angioplasty with stent. Acting quickly can save heart muscle—and your life.
How to lower this risk
You cannot remove the risk entirely, but you can cut it.
Work closely with your cardiologist to:
- Take blood thinners exactly as prescribed
- Never stop a heart medicine without medical advice
- Tell all your doctors and dentist about your stent
- Discuss any surgery or procedures planned in the next year
- Avoid smoking and manage diabetes, blood pressure, and cholesterol
Real‑life example:
A 62‑year‑old man stopped his blood thinners before a dental visit, without asking his cardiologist. Two weeks later, he had severe chest pain and a heart attack. A clot had formed in his stent. This kind of situation is often preventable with better communication.
For more detail on this topic, the Mayo Clinic information on coronary angioplasty and stents explains how stents work and why blood thinners matter.
2. Risk of Serious Bleeding From Blood Thinners 🩸
To prevent clots, you usually take at least two blood thinning medicines. These drugs are lifesaving, but they bring a bleeding risk.
Types of bleeding
Most bleeding episodes are minor, like:
- Easy bruising
- Nosebleeds
- Bleeding gums when brushing
However, some bleeding can be serious or even life threatening. For example:
- Vomiting blood or material that looks like coffee grounds
- Black, tar‑like stools
- Blood in urine
- Severe headaches or sudden vision changes
- Weakness on one side of the body
These may signal bleeding inside the stomach, intestines, or brain.
Balancing clot prevention and bleeding
Your cardiologist tries to balance two risks. Too little blood thinning increases clots. Too much increases bleeding.
They consider:
- Your age
- Past history of ulcers or bleeding
- Kidney and liver function
- Other medicines that affect bleeding
Sometimes, they choose a shorter course of strong blood thinners. Other times, you may need them for a year or longer.
How you can help protect yourself
You can play a big role in staying safe:
- Take your medicines at the same time every day
- Avoid over‑the‑counter pain pills like ibuprofen, unless cleared
- Limit alcohol, which can increase bleeding risk
- Report any unusual bruising or bleeding promptly
- Ask before taking new supplements or herbal remedies
Real‑life example:
A woman in her 70s started a new arthritis pain pill on her own. It interacted with her blood thinner and led to a stomach bleed. A quick call to her cardiologist first could have avoided this.
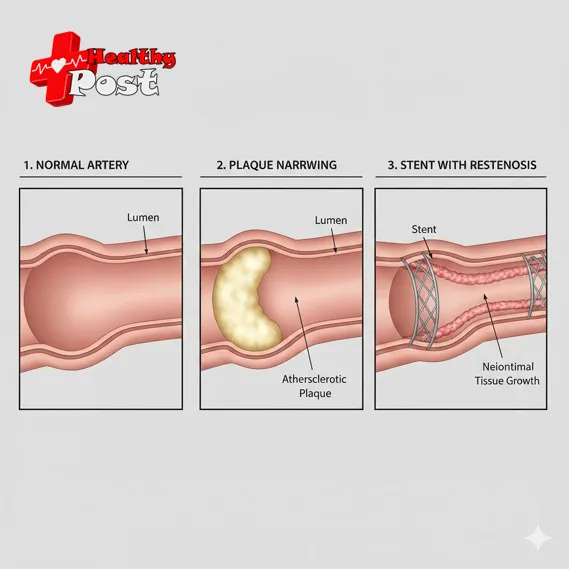
3. Risk of Restenosis: The Artery Narrowing Again 😟
Another risk of coronary stent surgery is restenosis, or the artery narrowing again. This risk has decreased with modern drug‑eluting stents, but it still happens.
Why arteries can re‑narrow
Over time, tissue can grow inside the stent. This growth can narrow the space for blood to flow.
Key reasons include:
- Very small artery size
- Long or multiple stents in the same vessel
- Uncontrolled diabetes
- Ongoing smoking
- Aggressive plaque build‑up
Symptoms of restenosis
Restenosis symptoms often feel similar to your original problem:
- Chest discomfort with exertion
- Shortness of breath on hills or stairs
- Tightness or pressure after emotional stress
- Fatigue out of proportion to activity
Do not dismiss these as “just getting older.” If symptoms return or worsen, contact your cardiologist.
Treatment options if it happens
If your doctor suspects restenosis, they may order:
- A stress test
- Imaging such as a CT coronary angiogram
- Repeat angiography with possible re‑stenting or other treatment
The best approach depends on:
- Which artery is involved
- How severe the narrowing is
- Your overall heart function
You can lower this risk by:
- Quitting smoking, if you smoke
- Managing blood sugar and blood pressure well
- Following a heart‑healthy eating pattern
- Staying active within your doctor’s advice
These lifestyle changes matter as much as the procedure itself. They support your stent and your entire circulation.
4. Risk of Allergic Reactions and Kidney Problems From Dye 💧
During angioplasty with stent, doctors use contrast dye so they can see your arteries on X‑ray. This dye is important, but it carries two main risks: allergic reactions and kidney injury.
Allergic reactions
Some people are sensitive to contrast dye. Symptoms can include:
- Itching or hives
- Swelling of lips, face, or tongue
- Wheezing or trouble breathing
Severe reactions are rare. Hospitals keep emergency medicines ready just in case.
To reduce risk, always tell your team if you have:
- A history of contrast dye allergy
- Asthma or many other allergies
Your doctor may give you pre‑treatment medicines to prevent reactions.
Kidney strain or injury
The kidneys help clear the dye from your body. If your kidneys are already weak, the dye can stress them further. In some cases, this leads to contrast‑induced kidney injury.
Risk is higher if you:
- Have chronic kidney disease
- Are older
- Have diabetes, especially if poorly controlled
- Are dehydrated or on certain medicines
Protecting your kidneys
Your team may:
- Check kidney function before the procedure
- Use the lowest safe amount of dye
- Give IV fluids to protect your kidneys
- Adjust or pause some medicines around the procedure
You can help by:
- Drinking fluids as advised before and after
- Avoiding non‑essential pain pills that strain kidneys
- Following all pre‑procedure instructions closely
5. Risk of Emotional Stress and False Sense of Security 😔
This risk is often overlooked but very real. After coronary stent surgery, many people expect to feel “fixed” and worry‑free. When that does not happen, emotional strain can grow.
Emotional reactions after stent placement
Common feelings include:
- Anxiety about every chest sensation
- Fear of another heart problem
- Sadness or frustration over health limits
- Anger about needing a procedure at all
Depression and anxiety are more common after heart procedures. They can even affect recovery and follow‑through with treatment.
False sense of security
Some people swing the other way. They feel the stent has “cured” their heart disease. They may:
- Return to smoking
- Ignore diet and exercise advice
- Skip follow‑up appointments
- Stop medicines on their own
This can be dangerous. A stent treats a specific blockage. It does not erase the underlying disease in your arteries.
How to support your emotional recovery
Protecting your heart also means protecting your mental health. Helpful steps include:
- Ask your doctor what to expect after the procedure
- Share your fears openly with your care team
- Join a cardiac rehabilitation program if offered
- Talk with a counselor if anxiety or sadness lingers
- Involve family so they understand your needs
Real‑life example:
A 55‑year‑old woman felt guilty and anxious after her stent. She avoided exercise out of fear. After joining cardiac rehab, she learned safe activity levels and felt more confident. Her mood and stamina improved together. 💪
Common Warning Signs After a Stent: What to Watch
The table below summarizes some symptoms after stent placement and how urgent they might be. This is not a full list, but it can guide you.
| Symptom or Sign | Possible Meaning | Suggested Action |
|---|---|---|
| Mild bruising at wrist or groin | Normal effect of procedure and meds | Monitor at home |
| Small lump at catheter site | Local swelling or small hematoma | Call your doctor if it grows or hurts |
| Increasing pain, large swelling, or warmth at catheter site | Possible infection or large bleed | Call your doctor the same day |
| New chest pain or tightness | Possible heart problem or restenosis | Call emergency services immediately |
| Sudden severe shortness of breath | Possible heart or lung issue | Call emergency services immediately |
| Black or bloody stools, vomiting blood | Possible internal bleeding | Seek urgent care or emergency help |
| Sudden weakness, facial droop, or trouble speaking | Possible stroke | Call emergency services immediately |
When in doubt, it is safer to call for help than to wait.

FAQs About the Risks of Coronary Stent Procedures ❓
1. Is coronary stent surgery safe overall?
For most patients, the benefits outweigh the risks. The procedure is common and usually very successful. However, any heart intervention carries danger. That is why informed consent and close follow‑up are so important.
2. How long do I need to take blood thinners after my stent?
It depends on your stent type, heart history, and bleeding risk. Many people need dual therapy for 6–12 months. After that, they often stay on a single blood thinner long term. Only your cardiologist can set your exact plan.
3. Can lifestyle changes reduce my risk of complications?
Yes, lifestyle plays a huge role. Not smoking, eating a heart‑healthy diet, staying active, and managing stress all help. These steps reduce restenosis risk and protect other arteries too.
4. How do I know if my chest pain after a stent is serious?
Treat new, intense, or clearly changing chest pain as an emergency. Especially if it comes with nausea, sweating, or breathlessness. It is safer to be checked and told it is not your heart than to delay.
5. Will I need another stent in the future?
Some people never need another stent. Others develop new blockages over time. Your risk depends on genetics, lifestyle, and other conditions. Regular follow‑up and preventive care lower the chance of future procedures.
6. Are there alternatives to a stent?
Sometimes medicines alone or bypass surgery are options. The best choice depends on how many arteries are blocked and where. A detailed talk with your cardiologist can compare these options for your specific case.
Conclusion: Turning Risk Awareness Into Heart Protection 💚
Understanding the risks of coronary stent surgery does not mean rejecting it. Instead, it helps you partner with your care team. You can ask sharper questions, spot warning signs earlier, and protect your long‑term health.
We covered five key risk areas:
- Clots forming inside the stent
- Bleeding from blood thinners
- Restenosis, or the artery narrowing again
- Allergic reactions and kidney stress from contrast dye
- Emotional strain and a false sense of security
Each risk has ways to reduce it. These include taking medicines exactly as prescribed, reporting symptoms early, and embracing heart‑healthy habits. Regular follow‑up visits are not just routine. They are a safety net.
Before you agree to coronary stent surgery, share your questions, fears, and health history honestly. After the procedure, stay engaged, informed, and supported. With knowledge, teamwork, and healthy daily choices, a stent can be one important tool in a much bigger plan to protect your heart. 🌿

