
How Outsourcing Orthopedic Billing Improves Revenue Cycle Management?
Managing billing for an orthopedic practice can be a real headache especially when you’re already busy caring for patients. From insurance rules to claim denials and delayed payments, the billing process often feels confusing and frustrating.
That’s why many orthopedic providers are now turning to outsourcing as a smarter solution. But how exactly does outsourcing orthopedic billing help? And can it really improve your Revenue Cycle Management (RCM)?
In this blog, we’ll walk you through everything in the simplest way possible, including what RCM is, the problems with in-house billing. And how outsourcing can boost your income, reduce stress, and keep your practice running smoothly.
What is Revenue Cycle Management in Healthcare?
Revenue Cycle Management (RCM) is the process that helps medical practices and hospitals get payments for the services they provide. Basically, it includes every step involved in managing a patient’s account. It starts from the moment they schedule an appointment until the final payment is received.
Why is RCM Important?
Firstly, think of RCM as the financial backbone of a healthcare practice. Because if it doesn’t run smoothly, the practice can lose money and even struggle to stay open. A strong RCM system ensures that the clinic gets fees on time and in full, without unnecessary delays or denials.
Key Stages of Revenue Cycle Management
- Patient Registration
This is the first step where patient details like insurance information and medical history are collected. Also, accurate data entry here sets the stage for the rest of the process.
- Medical Coding and Charge Entry
After the doctor sees the patient, the visit is documented and converted into medical codes. Hence, these codes explain what services were provided and are used to create the bill (claim).
- Billing and Claim Submission
Moving on, the bill is sent to the patient’s insurance company. It’s critical that the claim is accurate because, even small mistakes can cause delays or denials.
- Payment Processing and Collections
Finally, once the claim is approved, the insurance company sends payment. And any remaining balance is then billed to the patient. Also, timely follow-up is essential to ensure full payment.
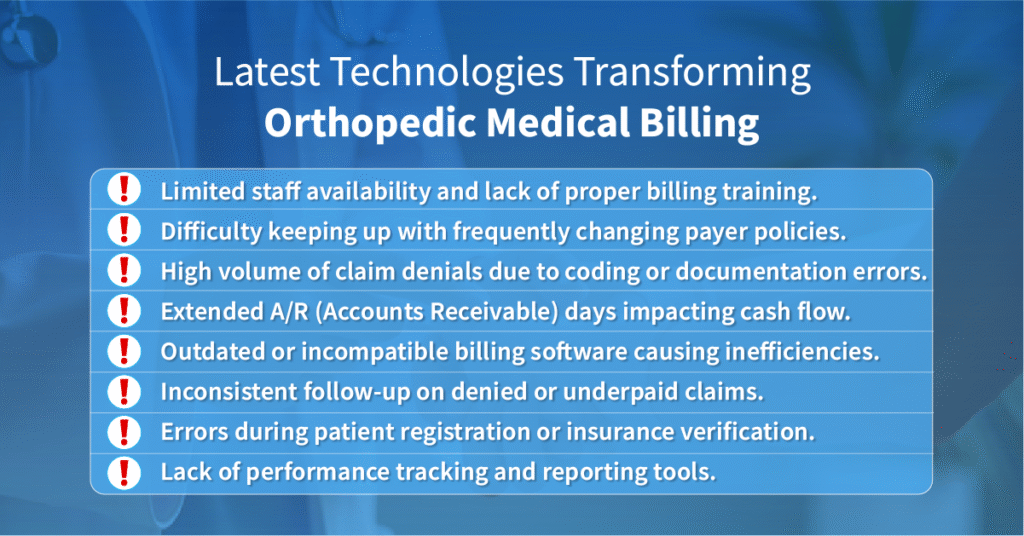
Where Things Go Wrong — and Cost You Money
Many medical practices lose money due to following reasons:
- Errors in patient information or coding
These lead to claim rejections or denials.
- Delayed claim submission
Waiting too long to file a claim can result in missing deadlines and lost payments.
- Lack of follow-up on denied or underpaid claims
Without proper tracking, denied claims often go unpaid.
- Inadequate staff training or high turnover
Mistakes are more common when the billing team lacks proper knowledge.
Pro Tip: When RCM isn’t handled properly billing is not the only thing it affects. It also directly impacts how much money your orthopedic practice brings in.
Outsourcing vs. In-House: A Quick Comparison Table
| Feature | In-House Billing | Outsourced Billing |
| Expertise Level | Depends on staff training and experience | Expert team with orthopedic billing expertise |
| Staffing & HR Costs | High. It includes hiring, salaries, benefits, training | Lower. It is handled by the billing company |
| Claim Accuracy | Varies. It is more prone to manual errors | High! claims are double-checked with latest tools |
| Denial Management | Often delayed or inconsistent | Proactive and systematic follow-up on all denials |
| Technology & Software | May rely on outdated or limited tools | Uses updated, industry-grade billing systems |
| Scalability | Hard to scale quickly with limited staff | Easily scalable with on-demand resources |
| Compliance & Updates | Requires regular internal training | Handled by certified experts who stay up-to-date |
| Cash Flow Speed | Slower due to delays and errors | Faster claim submission and quicker reimbursements |
| Focus | Divided between billing and care | Full focus on patients. Billing is off your plate! |
| Overall Cost | Higher in the long run due to overhead and inefficiencies | Cost-effective and revenue-boosting |
How Outsourcing Streamlines the Entire RCM?
If you run or manage an orthopedic practice, you already know that billing and revenue management can be frustrating, confusing, and also time-consuming. And when things don’t go the right way, like delayed payments or denied claims your practice loses money.
Now let’s break down outsourcing orthopedic billing. So you fully understand how it improves every step of your revenue cycle. And why it might be the smartest decision for your orthopedic practice.
1. You Get a Team of Specialists Without Hiring Them
Firstly, handling orthopedic billing in-house often means relying on a small team. Or sometimes there is even one person to manage a complex process.
But, orthopedic billing is highly specialized. It involves tough medical codes, surgical procedures, and payer-specific rules that constantly change.
On the contrary, when you outsource, you’re not just hiring one person, you’re getting a team of trained billing professionals. And they already know:
- Know the ins and outs of orthopedic procedures
- Stay up-to-date with changing insurance and Medicare/Medicaid policies
- Follow strict quality control and compliance standards
In addition, this level of expertise is hard (and expensive) to build internally. But, outsourcing allows you to access it right away.
2. Reduces Billing Errors and Claim Denials
One of the biggest reasons practices lose money is because of incorrect or incomplete claims. Often, small errors like a wrong CPT code or missing modifier can lead to denials, rework, or payment delays.
On the other hand, outsourced billing companies have error-checking systems in place. They:
- Review each claim for accuracy before submission
- Use the correct codes for orthopedic-specific procedures
- Catch issues early to avoid rejections
As a result, your claims get paid the first time, and you avoid the time and hassle of resubmitting.
3. Faster Claim Submission and Quicker Payments
Time is money in healthcare billing. If claims are delayed, your revenue is delayed. Because of this an outsourcing company works on a set schedule with a dedicated team, which means:
- Claims are submitted daily or weekly without delays
- Reimbursements come in faster
- There’s a constant flow of revenue into your practice
They also use automated tools and RCM software to speed up the entire cycle, from charge entry to payment posting.
4. You Avoid Staffing Issues and High Turnover
Let’s face it: billing staff can leave, go on vacation, or need training. Hiring and training new employees takes time and money, and your revenue suffers during the transition.
But with outsourcing, there’s no disruption in your billing process, ever!
You don’t have to:
- Worry about HR headaches
- Spend money on training
- Cover for someone being out sick
The billing company ensures continuous support and consistent results.
5. You and Your Team Can Focus on What Matters. Patient Care!
If you’re spending time fixing claim denials, chasing payments, or managing billing staff, that’s time taken away from your patients.
On the other hand, outsourcing your RCM, you free up your internal team to focus on:
- Delivering excellent patient care
- Improving patient satisfaction
- Growing your practice
Billing stress would no longer be your problem, it becomes theirs.
6. You Get Real-Time Reports and Financial Insights
Outsourced billing partners don’t just submit claims and disappear. They provide detailed reporting and analytics that help you understand:
- Your collection rates
- Your most common denials
- What’s working and what’s not
As a result, these reports help you make smarter business decisions and improve your financial health over time.
7. Better Compliance and Reduced Risk
Billing mistakes don’t just cost you money, they can also lead to compliance risks, audits, or fines. Professional billing companies are trained to stay compliant with:
- HIPAA regulations
- Payer-specific rules
- CMS billing updates
Also, they help protect your practice from billing fraud, coding mistakes, and legal trouble.
Outsource your Orthopedic Billing. Result: Stronger Revenue. More Control. Less Stress.
At the end of the day, your goal is simple, you want to get paid for the services you provide quickly, fully, and without hassle.Outsourcing helps you:
Key Benefits of Outsourcing Orthopedic Billing
✅ Access to certified orthopedic billing experts without hiring in-house staff
✅ Fewer claim denials thanks to accurate coding and thorough quality checks
✅ Faster claim submissions and quicker reimbursements from payers
✅ Improved cash flow and more consistent monthly revenue
✅ No need to manage or train billing staff internally
✅ Always stay updated with changing payer policies and regulations
✅ Reduced administrative workload so you can focus on patient care
✅ Scalable solutions that grow with your practice
✅ Transparent reporting and performance insights for smarter decisions
Conclusion
Orthopedic billing is not just paperwork, it directly affects how much money your practice earns and how smoothly it runs. As you’ve seen throughout this guide, managing billing in-house comes with many challenges. For instance, starting from claim errors and staff issues to slow payments and financial stress.
When these problems pile up, they can hurt your revenue and take your focus away from patient care. That’s why outsourcing is becoming the smart choice for many orthopedic practices.
In addition, with a team of billing experts, advanced tools, and faster processes, outsourcing helps you improve everything. For example, claim accuracy, reduce denials and speed up payments, all while lowering costs and saving time.
Most importantly, it gives you and your team extra time, so you can focus on your primary tasks. Finally, if you want fewer billing problems, more financial control, and steady practice growth, then outsourcing your orthopedic billing might be exactly what you need.

One thought on “How Outsourcing Orthopedic Billing Improves Revenue Cycle Management?”