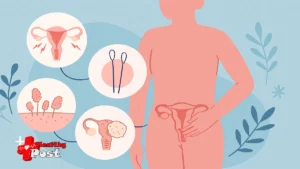
7 Powerful Reasons a Pap Smear Is Essential (What Is a Pap Smear & Tool Explained)
Sitting in a waiting room for a gynecology appointment can feel nerve‑wracking.
Maybe you are wondering what will happen during the exam.
Maybe you delayed scheduling for months or even years.
You are not alone. Many women feel anxious about a pap smear.
Understanding the test, the tools, and the reasons it matters can ease that fear.
This article explains:
- What happens during the test
- How the pap smear tool works
- Seven life‑protecting reasons to stay up to date
- Common worries, answered with compassion and facts
Let’s walk through it step by step, so you feel informed and in control. 😊
1. Understand What the Test Is Actually Checking 🩺
Before talking about benefits, it helps to answer what is a pap smear.
Knowing this can make the entire experience less frightening.
A Pap test is a screening exam for the cervix.
The cervix is the lower, narrow part of the uterus.
It connects the uterus to the vagina.
During the test, a clinician collects a small sample of cells.
These cells come from the surface of your cervix.
The sample is then examined under a microscope in a laboratory.
Specialists look for:
- Abnormal cells that might become cancer
- Early cell changes caused by high‑risk HPV types
- Inflammation or infection clues, in some cases
The test itself does not diagnose cancer by itself.
Instead, it spots suspicious changes very early.
That early warning allows treatment before cancer forms.
A trusted explanation of what is a pap smear is also available from Mayo Clinic.
What happens during the appointment
Here is a simple walk‑through of a typical visit:
- You undress from the waist down.
- You lie on an exam table with your feet in supports.
- The clinician gently inserts a speculum into the vagina.
- The speculum opens slightly, so the cervix is visible.
- A small brush collects cells from the cervix surface.
- Sometimes a tiny spatula collects cells from the canal.
- The tools are removed and the sample goes to the lab.
Most people feel pressure, not sharp pain.
The entire collection usually takes less than one minute.
🧡 Real‑life example:
Maria postponed her screening for four years.
She imagined the exam would be very painful.
Her doctor walked her through each step calmly.
The test felt uncomfortable but quick, and she felt relieved afterward.

2. It Finds Cell Changes Long Before Cancer Develops 🧬
The biggest strength of this test is timing.
It can detect abnormal cells years before they turn into cancer.
Cervical cancer usually develops slowly.
Cells move through stages:
- Healthy cells
- Mild changes
- Moderate or severe changes
- Precancer
- Invasive cancer
A Pap test often detects problems in the “changes” or “precancer” stages.
Treatment at these stages is typically very effective.
Procedures are usually less invasive and have better outcomes.
Why early detection matters
Cervical cancer detected early is highly curable.
When cancer is found late, treatment becomes more complex.
Early detection can mean:
- Less aggressive procedures
- Shorter recovery times
- Lower risk of long‑term complications
- Higher chance of cure
Regular screening gives your healthcare team a timeline.
They can watch for any small shifts from normal to abnormal.
HPV and Pap testing
Most cervical cell changes are linked to HPV.
HPV stands for human papillomavirus.
Some key points:
- HPV is very common and usually silent.
- Many sexually active people will catch HPV at some point.
- Most infections clear on their own.
- A small number cause persistent changes in cervical cells.
The Pap test looks for those cell changes.
Sometimes an HPV test is done at the same time.
Your clinician may suggest co‑testing depending on your age.
3. The Pap Smear Tool Is Designed for Safety and Precision 🛠️
Many people feel nervous about the instruments used.
Knowing how the pap smear tool works can ease that concern.
During the exam, your clinician may use:
- A speculum
- A cervical brush
- A small plastic spatula
- A collection container with liquid
These tools are simple but effective.
They are designed to collect cells gently and safely.
The main tools and what they do
Here is a quick guide to the tools used during a Pap test:
| Tool | What it Looks Like | What it Does | Comfort Tips |
|---|---|---|---|
| Speculum | Smooth, duck‑bill shaped device | Holds the vaginal walls apart | Slow breaths help reduce tension |
| Cervical brush | Small brush with soft bristles | Gently brushes cells from the cervix surface | The brushing is brief |
| Plastic spatula | Thin, flat plastic piece | May collect cells from around the cervical opening | Usually feels like light scraping |
| Collection vial with liquid | Small test tube with clear fluid | Holds the collected cells for lab analysis | You do not feel this step |
Modern devices are tested for safety and quality.
Clinicians learn specific techniques to reduce discomfort.
Authoritative details about the pap smear tool and procedure are summarized by the American College of Obstetricians and Gynecologists.
Ask for adjustments
You can always speak up during the exam.
You may ask for:
- A smaller speculum
- Extra lubricant if appropriate
- A pause if you feel anxious
- Step‑by‑step explanations during each move
Your comfort is part of your care.
A respectful clinician will welcome your questions.
🧡 Real‑life example:
Tara had a painful first pelvic exam.
At her next visit, she told her new doctor.
They used a smaller speculum and went slowly.
Her experience felt manageable and far less stressful.

4. It Gives You a Clear Screening Schedule and Plan 📅
Another powerful benefit of this test is structure.
It helps anchor your broader reproductive health routine.
Guidelines vary slightly by country and organization.
Always follow the advice of your own clinician.
Still, general patterns are similar.
Typical screening patterns by age
Use this table as a general guide only.
Your personal schedule may differ.
| Age Range | Typical Approach* | Notes |
|---|---|---|
| Under 21 | Usually no cervical screening | Even if sexually active |
| 21–29 | Pap test every 3 years | If results remain normal |
| 30–65 | Pap test every 3 years, or co‑testing every 5 years | Co‑testing combines Pap and HPV testing |
| Over 65 | Many can stop screening | If long history of normal results |
| After hysterectomy | Depends on reason for surgery | Ask if you still need cervical screening |
*These are general recommendations, not personal medical advice.
Regular screening creates a rhythm.
You can combine visits with other preventive checks.
For example, during the same visit, your provider may:
- Review contraception options
- Discuss menstrual issues
- Screen for sexually transmitted infections
- Address pelvic pain or vaginal symptoms
Your appointment becomes a holistic conversation, not only a lab test.
5. It Supports Fertility and Pregnancy Planning 🤰
Many people think only about cancer prevention.
However, cervical health also affects fertility and pregnancy.
Abnormal cells and untreated infections can sometimes cause issues.
While not every change affects fertility, knowing early is helpful.
How cervical health connects to future plans
Healthy cervical tissue helps:
- Sperm travel through the cervix to the uterus
- The cervix function properly in pregnancy
- Reduce risk of some pregnancy complications
When abnormalities are found early, treatments are usually conservative.
Your clinician will balance treatment goals with future fertility plans.
For example:
- Mild cell changes may only need monitoring.
- Moderate changes may need a minor procedure.
- Many treatments preserve the uterus and future fertility.
Discuss your pregnancy hopes before any procedure.
Your doctor can explain how treatments may affect those plans.
🧡 Real‑life example:
Nadia wanted children within a few years.
Her screening showed moderate cell changes.
Her gynecologist chose a targeted procedure.
They preserved her fertility and cleared the abnormal cells.
6. It Empowers You to Notice and Report Symptoms Sooner 🧠
Regular screening appointments train you to watch your own health.
You become more aware of what is normal for your body.
Each year or every few years, you check in with a professional.
You can share any new symptoms, even between tests.
Symptoms to report promptly include:
- Bleeding between periods
- Bleeding after sex
- Unusual or foul‑smelling discharge
- Pelvic pain or pressure
- Pain during intercourse
These symptoms do not always mean cancer.
They may reflect infections, fibroids, or hormonal changes.
Still, they always deserve attention.
The screening visit creates a safe space for discussion.
You can ask questions without feeling rushed or judged.
Over time, this builds health confidence.
You start to trust your body’s signals and your own voice.

7. It’s a Simple Step That Protects the People Who Love You ❤️
Many women care for others before themselves.
Children, partners, parents, and friends often come first.
Yet your health forms the foundation for all that caregiving.
Taking time for screening protects your own future.
It also supports the people who depend on you.
Think of this test as an act of self‑respect.
It says, “My life and health matter.”
Overcoming fear and embarrassment
Common worries include:
- “I am embarrassed to be examined.”
- “I am afraid it will hurt.”
- “I do not want to hear bad news.”
These feelings are understandable.
You can still move forward while feeling nervous.
Helpful approaches:
- Tell the clinician you feel anxious.
- Bring a trusted friend to the clinic.
- Practice slow breathing before and during the exam.
- Ask for clear explanations at each step.
Most people say the anticipation feels worse than the test.
Afterward, many feel proud they followed through.
Frequently Asked Questions ❓
1. Does the test hurt?
Most people feel pressure and brief discomfort.
Sharp pain is uncommon.
Tension can increase discomfort.
Slow, deep breaths can help your muscles relax.
Ask your clinician to pause if needed.
2. How often should I get screened?
It depends on your age, history, and test results.
Many guidelines suggest every three years for some adults.
Others allow longer intervals with HPV co‑testing.
Your doctor will recommend a schedule tailored to you.
3. Can I have the test during my period?
Light spotting may be acceptable.
Heavy bleeding can affect the sample quality.
If your period is very heavy, call the clinic.
They can tell you whether to keep or move the appointment.
4. Do I still need screening after HPV vaccination?
Yes, in most cases.
The HPV vaccine protects against several high‑risk virus types.
It does not cover every single possible type.
You still need regular cervical screening unless advised otherwise.
5. Can I refuse or delay the speculum exam?
You always have the right to consent or refuse.
If you feel unsafe or triggered, share that openly.
Some trauma‑informed clinicians offer extra support strategies.
Delaying indefinitely is not ideal, but your comfort matters.
6. What if my results come back “abnormal”?
An abnormal result does not mean you have cancer.
It usually means cell changes need a closer look.
Your clinician might repeat the test or order a colposcopy.
They will explain each next step and its purpose.
Conclusion: A Small Test With a Big Impact 🌱
Understanding what happens during a pap smear can transform fear into informed choice.
You now know:
- What the test checks and why
- How the pap smear tool works
- How early detection protects your future health
- How this screening connects to fertility, pregnancy, and family life
If you have delayed your appointment, consider this your gentle nudge.
You deserve answers, reassurance, and protection.
Schedule your screening, write down your questions, and bring them with you.
Let your next visit be a conversation, not just a procedure.
Your body is worthy of care.
Your future self will thank you for taking this simple, powerful step today. 💜