What is vulvar itching , symptoms, risk of infection, treatment
Vulvar itching is a common symptom of vulvar infection.
Due to cultural reasons, when faced with diseases involving private parts, many people choose to delay treatment as long as possible or treat it on their own, which may cause the disease to worsen or recur.
Understanding the relevant knowledge can help us face it scientifically, reduce troubles, and avoid affecting the quality of life due to illness.
In addition to the most common bacteria, fungi, parasites, etc. may cause vulvar infections. Among them, vulvovaginal candidiasis (Candida vulvovaginitis, VVC), commonly known as candidal vaginitis, is a common fungal infection in gynecology.
1. What is Candida?
Candida is a fungus, which may sound unfamiliar, but when we mention “mold”, “Candida” and ” thrush “, everyone is more familiar with it. Candida is also called Candida. Thrush, a common oral mucosal disease in infants and young children , is also caused by this type of fungus. The most common of these is Candida albicans (Candida albicans).
Candida is very common and can be found in the normal flora of the oral cavity, vulva and other parts. However, unlike oral candidiasis , oral infection often occurs in people with an imperfect immune system or immunodeficiency, and is called an opportunistic infection. Infections in the vulva and vagina occur in women with normal immune function.
Normally, Candida does not cause any symptoms (asymptomatic colonization). However, when the vaginal environment changes (perhaps due to medications, injury, or changes in the immune system, for example), Candida can overgrow and cause symptoms.
2. Where did the infection occur?
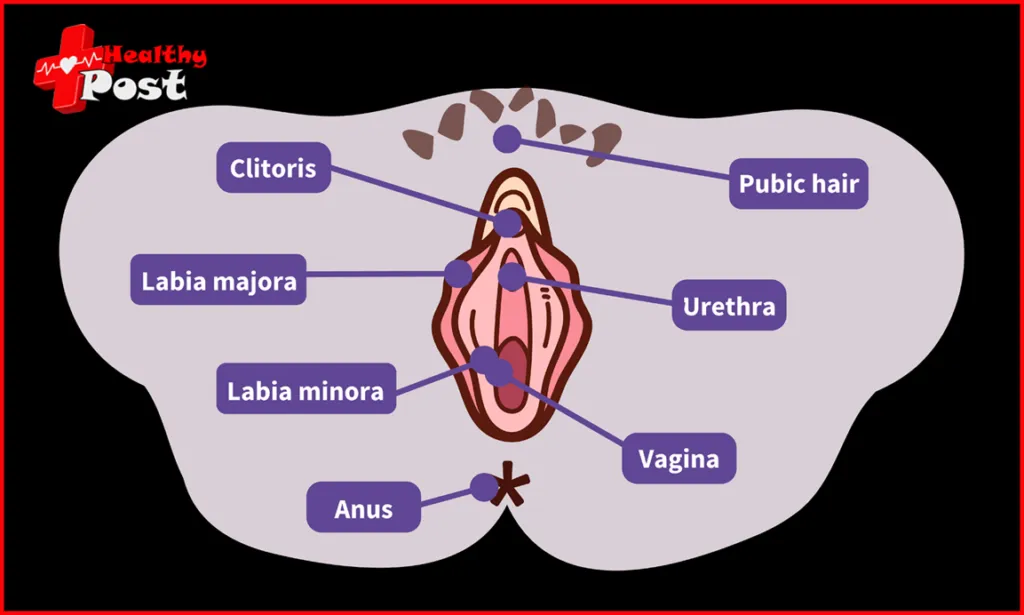
Since it is called vulvovaginal candidiasis (Candida vulvovaginitis), the infected areas are the vulva and vagina.
The picture below is a schematic diagram of the external genitalia (vulva) of an adult female . You can learn about the common structure and its relationship to the vagina, urethra, and anus, which will facilitate communication with the doctor during medical treatment or consultation.
3. How did you get infected?
The exact prevalence is difficult to determine because patients may self-treat, but it is estimated that 75% of women will have at least one episode of VVC in their lifetime, and 40% to 45% of women will experience two or more episodes [1].
If I take good care of my private parts, will I not get infected?
The mechanism of the transition from asymptomatic Candida colonization to symptomatic vulvovaginal disease is quite complex and involves host inflammatory responses and yeast pathogenic factors.
In daily life, we don’t need to take “special care” of the vulva, just clean it normally.
So if you find an infection, don’t worry about “why did I get infected when I was perfectly fine?” Scientific and reasonable treatment is the key.
❗ Pay attention to these risk factors
Although the mechanism of infection is complex, current studies have found that the following situations are prone to Candida infection.
- Diabetes: Women with type 2 diabetes may be more susceptible to non-albicans candidiasis .
- Use of antibiotics: The use of antibiotics increases the risk of infection because the normal bacterial flora is suppressed, which is beneficial to the growth of potential fungi (such as Candida). Therefore, it is necessary to weigh the pros and cons and use antibiotics rationally.
- Elevated estrogen levels: May occur more commonly in situations where estrogen levels are elevated, such as pregnancy and postmenopausal estrogen therapy.
- Immunosuppression: patients with immunodeficiency diseases (such as HIV infection) or those taking glucocorticoids or other immunosuppressive drugs.
- Genetics: Some studies have found that it is related to SIGLEC15 gene polymorphism.
There is still controversy as to whether oral contraceptives and contraceptive devices increase the risk of infection, and further research is needed.
Some people may wonder, if this is a vulvovaginal infection, is it a sexually transmitted infection (STI)?
Because Candida is a normal vaginal flora and the infection can occur in single women or women with no sexual life history or even young girls, it is usually not considered a sexually transmitted disease.
But this does not mean that Candida cannot be transmitted sexually, nor does it mean that vulvovaginal candidiasis is not related to sexual activity.
The impact of sexual behavior on the risk of Candida vulvovaginitis is still unclear [4], but some reports have found that the incidence of Candida vulvovaginitis increases in most women after they begin regular sexual activity. In addition, the strains colonizing infected women and their sexual partners are often the same.
4. What are the symptoms after infection?
When infection occurs, typical symptoms include vulvar itching (the most common, which can be manifested as vulvar itching and redness, swelling, cracks , and scratches), abnormal vaginal discharge (thick, curd-like discharge, commonly known as tofu-dreg leucorrhea), vaginal pain, dyspareunia, and vulvar itching and pain caused by urine irritation during urination [1-4].
Why do the symptoms differ for people who are all infected with Candida albicans?
Although the infection is mainly caused by Candida albicans, it can also be caused by other Candida species, such as Candida glabrata and Candida krusei.
Different Candida species can cause different symptoms and treatments. Therefore, when you have problems such as itching and abnormal discharge, you should not blindly use medication, but should identify the disease and the type of fungus that infects you and then treat it rationally.
5. How do you know if you are infected and how to treat it after infection?
When discomfort in the vulva or vagina occurs, the doctor will perform a physical examination and relevant laboratory tests. Such as vaginal discharge (leucorrhea) examination, to determine whether it is a Candida infection based on all the circumstances .
If it is a Candida infection, treatment includes oral and vaginal antifungal drugs (such as fluconazole capsules, clotrimazole vaginal tablets, etc.). But the specific choice of drugs and route of administration needs to be based on the specific condition. Whether you are pregnant, personal choice, etc., and should be use under the guidance of a doctor.
6. If I accidentally find that my leucorrhea is positive for Candida albicans, do I need to take medication?
Discovered incidentally, no treatment is required.
The 10% to 20% of women of childbearing age who carry Candida do not have symptoms and do not require treatment. Similarly, if Candida is found on a removed IUD, treatment is not required if there are no symptoms.
7. Do sexual partners need to be examined and/or treated after infection?
Not usually required.
However, for sexual partners with symptoms (such as balanitis), it is recommended to see a specialist for symptomatic treatment. If it is recurrent vulvovaginitis (≥3 times/year), there is still controversy about the treatment recommendations for sexual partners. Sexual partners may be recommended to be examined at the same time and given treatment if necessary.
8. What can be done to reduce the risk of infection?
Based on the information mentioned above, in addition to proper treatment after infection. We can start from the following points to reduce the risk of infection and discomfort:
- If you have diabetes, keep your blood sugar levels under control;
- Do not abuse antibiotics;
- Although sexual intercourse is not prohibited during infection, considering the possibility of dyspareunia during sexual intercourse. It is recommend to avoid sexual intercourse during the acute phase.
Do I need to wash my vagina? Do I need to change my clothes?
As mentioned earlier, we don’t need to provide “special care” to the vulva on a daily basis.
There is no evidence that vaginal douching can prevent or treat Candida infection.
The association between wearing tight-fitting or synthetic clothing and infection is weak and controversial between studies. So it is generally not necessary to change it.

9 thoughts on “What is vulvar itching , symptoms, risk of infection, treatment”