7 Alarming Signs Linked to Abdominal Tenderness ICD 10 Code Diagnosis
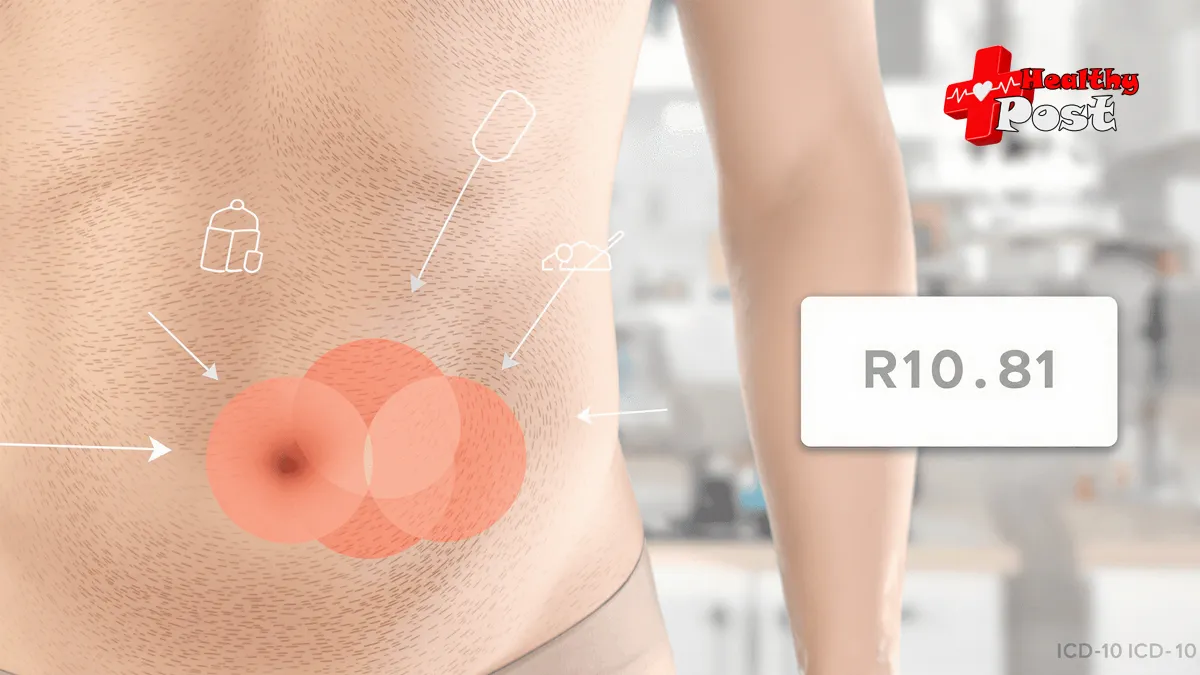
Abdominal tenderness is a key medical sign that helps doctors identify serious health issues. This symptom makes your belly feel sore when touched during a physical exam.
Your doctor needs to know the exact location and type of tenderness you feel. The ICD-10 code system helps track these details with code R10.81.
Think of abdominal tenderness as your body’s alarm system. It can point to:
- Simple digestive issues
- Serious infections
- Emergency conditions
- Chronic health problems
Getting the right diagnosis depends on spotting warning signs early. A proper medical code helps your healthcare team:
- Track your symptoms
- Plan your treatment
- Handle insurance claims
- Keep accurate health records
Did you know? Your belly pain could mean different things based on where it hurts and what other symptoms you have.
Let’s explore 7 warning signs that often appear with abdominal tenderness. These signs help doctors find the real problem behind your discomfort.
Learn more about abdominal pain diagnosis from Mayo Clinic
Understanding Abdominal Tenderness and Its Role in Diagnosis
Abdominal tenderness happens when your belly hurts when someone touches it during a check-up. Doctors check this by pressing different spots on your belly.
Key Signs of Abdominal Tenderness:
- Pain when the doctor presses your belly
- Discomfort when you move or cough
- A specific spot that hurts more than others
- Pain that gets worse when pressed
The abdominal tenderness icd 10 code R10.81 helps doctors track this symptom. This code belongs to a special list of medical codes doctors use.
Think of ICD-10 codes like a secret language doctors use to talk about health problems. Code R10.81 tells other doctors:
- The patient has belly pain when touched
- The exact spot of pain isn’t known yet
- More tests might be needed
Chapter 18 of ICD-10 (R00-R99) includes many belly-related symptoms. This chapter helps doctors when they:
- Need to record symptoms
- Haven’t found the main problem yet
- Want to track how symptoms change
Your doctor might use code R10.81 as a starting point. They’ll often need more tests to find out what’s causing your belly pain.
Common Tests After Finding Tenderness:
- Blood tests
- X-rays
- CT scans
- Ultrasound
These tests help doctors find the real reason behind your belly pain. The R10.81 code works like a first clue in solving a medical mystery.
Learn more about abdominal pain diagnosis
The location of your belly tenderness gives doctors important hints. Different spots can mean different problems:
- Upper right – might be gallbladder
- Lower right – could be appendix
- Upper middle – might be stomach issues
The Importance of Accurate Coding with ICD-10-CM Code R10.81
The non-billable code R10.81 serves as a vital documentation tool in medical records. This code helps track patient symptoms when a specific diagnosis hasn’t been determined yet.
Temporary Placeholder for Abdominal Tenderness
Medical providers use R10.81 as a temporary placeholder during the diagnostic process. It signals to other healthcare professionals that:
- The patient experiences abdominal tenderness
- A definitive diagnosis remains pending
- Additional tests or evaluations may be needed
Guiding Annotations for Precise Documentation
The code includes specific annotations that guide medical staff:
“Abdominal tenderness, unspecified site” – This indicates the need for more precise location documentation
Supporting Reimbursement Efforts
Healthcare facilities must maintain detailed records for reimbursement purposes. R10.81 helps by:
- Documenting initial symptoms
- Supporting medical necessity for ordered tests
- Creating a clear trail of diagnostic steps
Impacting Patient Care through Proper Coding
Proper coding impacts patient care through:
- Accurate medical history tracking
- Better communication between providers
- Appropriate treatment planning
- Streamlined insurance processing
Enhancing Documentation with Additional Symptoms
Healthcare providers should document additional symptoms alongside R10.81. This practice helps:
- Paint a complete clinical picture
- Support medical decision-making
- Enable proper insurance reimbursement
- Guide future treatment plans
Strengthening Records with Comprehensive Coding
The R10.81 code works with other diagnostic codes to create comprehensive medical records. This combination approach strengthens documentation quality and supports optimal patient outcomes.
1. Severe Abdominal Pain: A Red Flag for Serious Conditions
Severe abdominal pain is one of the most important signs that doctors look for when diagnosing serious conditions. This intense discomfort requires immediate medical attention because it may be a sign of a life-threatening issue.
Common Serious Conditions Associated with Severe Abdominal Pain:
- Appendicitis: Sharp pain starting near the belly button, moving to the lower right abdomen, and increasing with movement or coughing.
- Pancreatitis: Pain that radiates to the back, worsens after eating, and may cause nausea and vomiting.
- Gallbladder Disease: Upper right quadrant pain that often occurs after fatty meals and can cause fever and chills.
Doctors use specific codes to track these symptoms and understand what might be causing the pain:
R10.81: Abdominal tenderness R10.84: Generalized abdominal pain R10.13: Epigastric pain
Medical professionals use these codes to document:
- Pain location
- Pain intensity
- Associated symptoms
- Duration of symptoms
Different types of pain can indicate different conditions:
- Sudden sharp pain might mean there’s a perforation
- Cramping pain could suggest an obstruction
- Burning pain may signal ulcers
- Colicky pain often relates to gallstones
It’s crucial to seek medical help quickly when severe pain is accompanied by:
- Rigid abdomen
- Rebound tenderness
- High fever
- Rapid heart rate
These combined symptoms create a picture that helps doctors make accurate diagnoses and treatment plans.
2. Persistent Nausea and Vomiting: An Urgent Concern
Persistent nausea and vomiting paired with abdominal tenderness can signal serious digestive system problems. These symptoms often point to conditions that need quick medical help.
Common Serious Conditions Include:
- Bowel obstruction
- Intestinal perforation
- Severe gastritis
- Gastroparesis
- Inflammatory bowel disease
The presence of bile in vomit suggests a blockage past the stomach. Green or yellow vomit needs immediate medical care.
Key Warning Signs to Watch:
- Vomiting lasting more than 24 hours
- Unable to keep liquids down
- Blood in vomit
- Severe stomach pain
- Signs of dehydration
Healthcare providers face several challenges when diagnosing the root cause:
- Multiple Possible Causes: Infections, structural problems, medication side effects, chronic conditions
- Changing Symptom Patterns: Symptoms may come and go, pain levels can vary, nausea might worsen with movement
- Testing Limitations: Some tests require fasting, movement restrictions during imaging, time needed for lab results
Doctors often use a step-by-step approach to rule out life-threatening conditions first. They start with physical exams and blood tests before moving to specialized imaging.
Different vomiting patterns help narrow down possible causes. Projectile vomiting suggests different problems than regular nausea with occasional sick feelings.
The timing between eating and vomiting provides important clues. Food coming up right after eating points to different issues than delayed vomiting.
3. Unexplained Weight Loss: A Warning Sign Not to Ignore
Sudden weight loss paired with abdominal tenderness raises red flags for healthcare providers. A drop of 5% body weight within 6-12 months without trying signals potential health issues.
Common underlying conditions linked to unexplained weight loss include:
- Digestive system cancers
- Chronic inflammatory bowel disease
- Celiac disease
- Bacterial or parasitic infections
- Chronic pancreatitis
- Hyperthyroidism
The presence of abdominal tenderness with weight loss often points to digestive system problems. Your body might struggle to absorb nutrients properly, leading to unintended weight changes.
Healthcare providers look for specific patterns during physical examinations:
- Location of abdominal tenderness
- Changes in appetite
- Energy levels
- Digestive symptoms
- Sleep patterns
Early detection through proper medical evaluation can lead to better treatment outcomes. Your doctor may request:
- Blood tests to check inflammation markers
- Imaging studies of your digestive tract
- Endoscopic procedures
- Stool sample analysis
- Thyroid function tests
The combination of weight loss and abdominal tenderness requires immediate medical attention. These symptoms might reveal serious health conditions that need quick intervention.
A detailed medical history helps doctors identify the root cause. They’ll ask about:
- Recent lifestyle changes
- Family history
- Current medications
- Dietary habits
- Stress levels
Recording your symptoms and weight changes helps create an accurate diagnosis timeline. This information guides healthcare providers toward appropriate testing methods.
4. Change in Bowel Habits: A Clue Towards Diagnosis
Changes in bowel habits paired with abdominal tenderness serve as vital clues for precise documentation in medical diagnosis. These changes can range from:
- Sudden constipation
- Frequent diarrhea
- Alternating between both conditions
- Changes in stool consistency
- Unusual bowel movement timing
The presence of these symptoms alongside abdominal tenderness often points to specific digestive conditions. Many patients report discomfort or pain when touching their abdomen during these bowel changes.
Common Associated Conditions:
- Irritable Bowel Syndrome (IBS)
- Inflammatory Bowel Disease
- Celiac Disease
- Food Intolerances
- Bacterial Infections
Your healthcare provider might ask about specific patterns in your bowel movements:
- Frequency of movements
- Consistency of stool
- Time of day symptoms occur
- Related dietary triggers
- Duration of changes
These details help create an accurate diagnosis path. The ICD 10 code system uses this information to classify symptoms under specific categories.
Warning Signs to Watch:
- Blood in stool
- Black, tarry stools
- Severe cramping
- Uncontrollable urgency
- Nighttime symptoms
Tracking bowel habit changes helps doctors identify patterns. A detailed symptom diary can speed up the diagnostic process. This information guides healthcare providers toward appropriate testing and treatment options.
Proper documentation of these symptoms aids in creating a complete clinical picture. Your healthcare team uses this data to determine the root cause of abdominal tenderness.
5. Fever: An Indicator of Infection or Inflammation
A rise in body temperature often signals your body’s defense system at work. When abdominal tenderness comes with fever, it points to possible infection or inflammation inside your belly.
Your doctor will make special annotations in your medical records when fever appears with belly tenderness. These notes help track important changes in your condition.
Common causes of fever with abdominal tenderness include:
- Appendicitis
- Diverticulitis
- Gallbladder infection
- Urinary tract infections
- Stomach flu
The height of your fever can tell doctors important things:
Low-grade fever (100-101°F): May suggest mild infections
High fever (102°F+): Often points to serious infections needing quick treatment
Your immune system raises your body temperature to:
- Kill harmful germs
- Speed up healing
- Alert your body to fight infection
- Help antibodies work better
Doctors check these things when you have fever and belly tenderness:
- Where the tenderness hurts most
- How long you’ve had the fever
- Other symptoms you might have
- Your recent health history
- Any medicines you’re taking
Blood tests help doctors see if your white blood cell count is high. A high count usually means your body is fighting an infection.
Some belly infections need antibiotics or surgery. Quick treatment helps stop the infection from spreading to other parts of your body.
Learn more about fever patterns and their meanings
Comprehensive Assessment Techniques for Healthcare Providers
Healthcare providers use specific methods to check abdominal tenderness. A proper diagnosis needs both physical tests and special scans.
Physical Examination Steps:
- Light touch testing of the abdomen
- Deep pressure tests in different spots
- Checking for rebound tenderness
- Listening to bowel sounds with a stethoscope
- Looking for visible swelling or bruising
Key Imaging Studies:
- X-rays to spot blockages or trapped air
- CT scans for detailed organ views
- Ultrasound to check soft tissues
- MRI for complex cases
Medical teams also track vital signs during these checks:
- Blood pressure readings
- Heart rate changes
- Temperature patterns
- Breathing rate
Blood tests help find hidden problems:
- Complete blood count
- Liver function tests
- Pancreatic enzyme levels
- Infection markers
The doctor’s hands-on exam gives quick clues about the pain source. Each gentle press tells a story about what’s happening inside.
Patients need to share their full health history. Small details can point to big answers:
- Past surgeries
- Recent injuries
- Food allergies
- Current medications
These assessment steps create a clear picture. Each finding adds another piece to solve the medical puzzle.
A mix of old-school physical exams and modern technology gives the best results. This team approach helps find the right treatment path.
Conclusion
Abdominal tenderness signals potential health issues that need quick medical attention. The seven signs we discussed help identify serious abdominal conditions early.
Key points to remember:
- Severe abdominal pain needs immediate medical evaluation
- Persistent nausea with vomiting suggests urgent medical problems
- Unexplained weight loss requires thorough investigation
- Changes in bowel habits point to digestive system issues
- Fever indicates possible infection or inflammation
Your health matters – don’t wait to get help when these warning signs appear. Proper symptom documentation using ICD 10 codes helps doctors make accurate diagnoses.
“Listen to your body. Any persistent abdominal discomfort deserves medical attention.”
Healthcare providers use these signs to:
- Assess your condition
- Order appropriate tests
- Create effective treatment plans
- Track your progress
Remember: Early detection through proper diagnosis saves lives. If you notice any of these seven alarming signs with abdominal tenderness, seek medical care right away.
Your doctor will use the right ICD 10 codes to document your symptoms and provide the best possible care for your specific situation.
FAQs (Frequently Asked Questions)
What is abdominal tenderness and why is it significant in medical diagnosis?
Abdominal tenderness is a clinical finding characterized by pain or discomfort when the abdomen is touched. It is significant in medical diagnosis as it can indicate underlying conditions ranging from mild to serious, helping healthcare providers identify potential abdominal issues.
How does the ICD-10 code R10.81 relate to abdominal tenderness?
ICD-10 code R10.81 specifically represents abdominal tenderness within the ICD-10 classification system, particularly under Chapter 18 (R00-R99), which covers symptoms related to the abdomen. This coding aids in accurate documentation and diagnosis.
Why is accurate coding with ICD-10-CM code R10.81 important in managing abdominal tenderness?
Accurate coding using ICD-10-CM code R10.81 ensures detailed medical documentation essential for reimbursement purposes and facilitates appropriate medical care for patients presenting with abdominal tenderness, even though R10.81 is a non-billable code.
What are some alarming signs linked to abdominal tenderness that require immediate attention?
Seven alarming signs linked to abdominal tenderness include severe abdominal pain, persistent nausea and vomiting, unexplained weight loss, changes in bowel habits, fever indicating infection or inflammation, among others. Recognizing these signs can aid in timely diagnosis and treatment.
How do changes in bowel habits alongside abdominal tenderness assist in diagnosis?
Changes in bowel habits such as diarrhea or constipation combined with abdominal tenderness provide valuable diagnostic clues pointing towards conditions like irritable bowel syndrome (IBS) or other gastrointestinal disorders, emphasizing the need for precise documentation.
What comprehensive assessment techniques should healthcare providers use when evaluating patients with abdominal tenderness?
Healthcare providers should employ comprehensive assessment techniques including thorough physical examinations and relevant imaging studies to evaluate patients suspected of having abdominal conditions, ensuring accurate diagnosis and effective treatment planning.


One thought on “7 Alarming Signs Linked to Abdominal Tenderness ICD 10 Code Diagnosis”