10 Alarming Signs Linked to Amenorrhea ICD 10 in Women
The absence of menstrual periods, known as Amenorrhea ICD 10, affects millions of women worldwide. This condition disrupts the natural menstrual cycle, signaling potential underlying health concerns that require medical attention.
Medical professionals use the ICD-10 classification system to document amenorrhea cases accurately. This standardized coding system helps healthcare providers:
- Track patient diagnoses effectively
- Ensure proper insurance billing
- Facilitate communication between healthcare teams
- Guide appropriate treatment protocols
Women experiencing amenorrhea might face various health challenges, from hormonal imbalances to structural abnormalities. These 10 alarming signs can indicate serious medical conditions:
- Unexplained absence of periods
- Hormonal fluctuations
- Structural reproductive system anomalies
- Genetic variations
- Endocrine system disorders
- Pituitary gland dysfunction
- Ovarian conditions
- Hypothalamic issues
- Anatomical abnormalities
- Systemic health problems
Understanding these warning signs empowers women to seek timely medical intervention. Each sign provides valuable clues about potential underlying causes, helping healthcare providers determine appropriate diagnostic tests and treatment strategies.
This comprehensive guide explores these critical indicators, their significance, and their relationship to amenorrhea diagnosis under ICD-10 classification.
Understanding Amenorrhea and Its Types
Amenorrhea refers to the absence of menstrual periods during a woman’s reproductive years. This condition affects approximately 3-4% of women, impacting their reproductive health and potentially indicating underlying health issues.
Medical professionals classify amenorrhea into two distinct categories:
1. Primary Amenorrhea
This type of amenorrhea is diagnosed when:
- No menstrual periods occur by age 15
- Periods have not started within 5 years of breast development
Common causes of primary amenorrhea include:
- Genetic conditions
- Hormonal imbalances
- Anatomical abnormalities
2. Secondary Amenorrhea
Secondary amenorrhea is identified when:
- A woman experiences absence of periods for 3 or more consecutive months
- There is a previous history of regular menstruation
Common causes of secondary amenorrhea include:
- Pregnancy
- Breastfeeding
- Stress
- Extreme weight changes
- Hormonal disorders
The distinction between these types helps guide diagnostic approaches. Primary amenorrhea often indicates developmental issues requiring genetic testing, while secondary amenorrhea points to acquired conditions needing hormonal evaluation.
Both types can significantly impact fertility, bone health, and emotional well-being. A missed period might signal various health conditions ranging from simple lifestyle factors to complex endocrine disorders.
Women experiencing either type should seek medical evaluation. Early identification of the underlying cause enables appropriate treatment strategies and helps prevent potential complications.
The Role of ICD-10 in Diagnosing Amenorrhea
Medical professionals rely on ICD-10 code N91.2 for accurate classification of unspecified amenorrhea cases. This standardized coding system enables healthcare providers to:
- Document medical conditions with precision
- Facilitate insurance claims processing
- Track patient outcomes effectively
- Support clinical research initiatives
- Enable data analysis for population health
The Amenorrhea ICD 10 classification includes specific subcategories:
- N91.0 – Primary amenorrhea
- N91.1 – Secondary amenorrhea
- N91.2 – Unspecified amenorrhea
- N91.3 – Primary oligomenorrhea
- N91.4 – Secondary oligomenorrhea
These detailed codes help healthcare providers pinpoint exact diagnoses, leading to:
“Precise medical documentation enhances communication between healthcare providers, improves patient care coordination, and streamlines the billing process.”
The coding system integrates with electronic health records (EHR) systems, creating a standardized approach to:
- Clinical documentation
- Treatment planning
- Healthcare analytics
- Quality metrics reporting
- Population health management
Proper use of ICD-10 codes supports evidence-based medicine through accurate data collection. Healthcare providers can track treatment effectiveness, identify patterns, and develop targeted interventions for specific patient populations.
1. Müllerian Agenesis: A Genetic Cause of Primary Amenorrhea
Müllerian agenesis is one of the most significant genetic causes of primary amenorrhea, which is one of the 10 Alarming Signs Linked to Amenorrhea ICD 10 in Women. This rare congenital condition affects 1 in 4,500 female births, resulting in the absence or underdevelopment of the uterus and upper vagina.
Women with Müllerian agenesis have normal external genitalia and secondary sexual characteristics. The condition becomes apparent during adolescence when menstruation fails to begin, leading to primary amenorrhea.
Key Diagnostic Features:
- Normal ovarian function
- Typical female chromosome pattern (46, XX)
- Absent or rudimentary uterus
- Shortened vaginal canal
- Normal breast development
- Regular hormone levels
- Presence of functioning ovaries
Diagnosis
The diagnosis involves several medical evaluations:
- Physical examination
- Pelvic ultrasound imaging
- Magnetic resonance imaging (MRI)
- Hormone level testing
- Genetic testing
Treatment
Women with Müllerian agenesis maintain normal ovarian function, producing regular levels of female hormones. This explains their typical breast development and other secondary sexual characteristics. The condition specifically affects the development of the Müllerian ducts, which form the uterus, cervix, and upper vagina during fetal development.
Treatment options focus on creating a functional vaginal canal through non-surgical or surgical methods. Psychological support plays a vital role in helping patients cope with fertility implications and relationship concerns.
2. Androgen Insensitivity Syndrome: A Hormonal Disorder Behind Primary Amenorrhea
Androgen insensitivity syndrome (AIS) is a genetic condition that affects individuals with XY chromosomes. Despite having male chromosomes, these individuals develop female external characteristics.
Causes and Effects of AIS
The condition occurs because the cells in the body are unable to respond to androgens, which are male hormones necessary for male sexual development. As a result of this resistance:
- Female external genitalia develops
- Breast development occurs during puberty
- Body hair is absent or minimal
- Primary amenorrhea (absence of menstruation) is present
- Undescended testes are observed
Women with AIS have higher levels of testosterone compared to typical females, but their bodies are unable to utilize these hormones. The testes produce normal amounts of androgens, but the cells in the body lack functional androgen receptors.
Diagnosis of AIS
The diagnostic process for AIS involves several steps:
- Genetic testing to confirm the presence of XY chromosomes
- Blood tests to measure hormone levels
- Pelvic imaging techniques such as ultrasound or MRI to identify undescended testes
- Evaluation of family history to assess any potential genetic factors
Management Strategies for AIS
Managing AIS requires a comprehensive approach that addresses both physical and psychological aspects:
- Providing psychological support and counseling to affected individuals and their families
- Administering hormone replacement therapy to maintain hormonal balance
- Conducting regular monitoring of bone density to prevent osteoporosis
- Performing surgical removal of undescended testes if necessary
- Implementing vaginal dilation therapy when needed for sexual health
Importance of Early Diagnosis and Ongoing Care
Early diagnosis plays a crucial role in ensuring appropriate medical care and support for individuals with AIS. Healthcare providers must approach discussions about AIS with sensitivity and empathy, considering the emotional impact it may have on patients and their families.
Regular follow-up appointments are essential for monitoring hormone levels, addressing any potential complications, and providing ongoing support. A multidisciplinary team approach involving endocrinologists, psychologists, surgeons, and other specialists can help ensure comprehensive care for women with AIS.
3. Polycystic Ovary Syndrome (PCOS): A Common Cause of Secondary Amenorrhea
PCOS affects up to 10% of women worldwide, making it a leading cause of secondary amenorrhea. This complex hormonal disorder disrupts the normal menstrual cycle through hormonal imbalances.
Symptoms of PCOS
Women with PCOS may experience:
- Irregular or absent periods
- Multiple small cysts on ovaries
- High levels of male hormones (androgens)
- Insulin resistance
- Difficulty managing weight
How is PCOS Diagnosed?
Medical professionals use the Rotterdam criteria to diagnose PCOS. A patient must present with at least two of these conditions:
- Irregular or absent menstruation
- High androgen levels or physical signs of excess androgens
- Polycystic ovaries visible on ultrasound
Treatment Options for PCOS-related Secondary Amenorrhea
Treatment plans for PCOS-related secondary amenorrhea include:
- Birth control pills to regulate menstrual cycles
- Anti-androgen medications
- Metformin for insulin resistance
- Lifestyle modifications:
- Regular exercise
- Balanced diet
- Stress management techniques
- Weight control strategies
Blood tests help monitor hormone levels during treatment, while regular ultrasounds track changes in the ovaries and progress of the treatment. Early intervention is crucial in reducing long-term health risks associated with PCOS, such as diabetes and cardiovascular disease.
4. Hypothalamic-Pituitary Dysfunction: An Underlying Factor in Secondary Amenorrhea Cases
Hypothalamic-pituitary dysfunction is a significant cause of secondary amenorrhea, affecting the delicate hormone balance essential for menstruation. This condition disrupts the communication between the hypothalamus and pituitary gland, leading to a series of hormonal imbalances that can halt menstruation.
Common Triggers of Hypothalamic Dysfunction:
- Excessive exercise or athletic training
- Significant weight loss or eating disorders
- Chronic stress
- Severe illness
- Head trauma
The hypothalamus releases GnRH (Gonadotropin-Releasing Hormone) in specific pulses. Any disruption to these pulses can halt menstruation. This disruption creates a chain reaction affecting hormone production throughout the body.
Key Diagnostic Indicators:
- Low levels of luteinizing hormone (LH)
- Reduced follicle-stimulating hormone (FSH)
- Decreased estrogen production
- Normal prolactin levels
- Absence of other medical conditions
Treatment focuses on addressing the underlying cause:
- Weight restoration in cases of eating disorders
- Stress management techniques
- Modification of exercise routines
- Hormone replacement therapy when necessary
- Regular monitoring of hormone levels
A comprehensive medical evaluation helps identify specific triggers. Brain imaging through MRI can rule out structural abnormalities, while blood tests track hormone levels and guide treatment adjustments.
Successful management requires patience and consistent monitoring. Many patients regain regular menstruation once the underlying cause receives proper treatment.
For further understanding, you may explore more about hypothalamic-pituitary dysfunction and its impact on menstrual health. Additionally, insights into diagnostic indicators and treatment options for this condition are available in these resources.
5. Hyperprolactinemia: A Hormonal Imbalance Linked to Secondary Amenorrhea
Hyperprolactinemia disrupts the normal menstrual cycle by elevating prolactin levels in the blood. This hormonal imbalance affects up to 10% of women with secondary amenorrhea.
The condition interferes with the production of essential reproductive hormones:
- Reduces GnRH secretion
- Decreases FSH levels
- Lowers LH production
- Suppresses estrogen synthesis
Common Causes of Hyperprolactinemia:
- Pituitary tumors (prolactinomas)
- Certain medications
- Thyroid disorders
- Chronic stress
- Pregnancy and breastfeeding
Women with hyperprolactinemia often experience these symptoms:
- Irregular or absent periods
- Unexplained milk production
- Headaches
- Vision changes
- Decreased libido
Diagnostic Approach:
- Blood prolactin level testing
- MRI of the pituitary gland
- Thyroid function assessment
- Medication review
Treatment options vary based on the underlying cause:
- Dopamine agonist medications
- Surgical removal of prolactinomas
- Adjustment of current medications
- Management of thyroid conditions
- Stress reduction techniques
Regular monitoring of prolactin levels helps track treatment effectiveness. Most women resume normal menstrual cycles once prolactin levels return to normal range.
Identifying Alarming Signs Associated with Amenorrhea
Physical signs are crucial in diagnosing conditions related to amenorrhea. By carefully examining these signs, healthcare providers can determine the best treatment options.
Key Physical Signs to Monitor:
1. Breast Development Status
- Absent breast tissue suggests hormonal imbalances
- Asymmetrical breast development indicates potential endocrine disorders
- Underdeveloped breasts point to possible estrogen deficiency
2. Pubic Hair Patterns
- Complete absence might signal androgen insensitivity
- Sparse growth suggests hormonal irregularities
- Excessive hair growth indicates potential PCOS
Additional Warning Signs:
- Unexplained weight changes
- Skin changes or acne
- Voice deepening
- Headaches
- Vision changes
- Unusual breast discharge
- Facial hair growth
These physical signs often correspond to specific underlying conditions. Regular self-monitoring can help identify changes early on. Healthcare providers use these signs along with medical history to determine which diagnostic tests are necessary.
A thorough physical examination can provide valuable insights into the underlying cause of amenorrhea. Keeping track of any changes in these signs can help detect serious conditions at an early stage.
Evaluating Hormonal Factors in Diagnosing Amenorrhea Cases
Hormone level analysis is a crucial diagnostic tool for identifying the underlying causes of amenorrhea. A comprehensive hormonal evaluation includes:
- Estrogen Levels: Low estrogen can signal ovarian dysfunction or hypothalamic issues
- FSH and LH Testing: Elevated levels might indicate primary ovarian insufficiency
- Thyroid Function: Abnormal thyroid hormones can disrupt menstrual cycles
- Prolactin Measurement: High levels suggest potential pituitary tumors
- Testosterone Analysis: Elevated readings point to possible PCOS or adrenal disorders
Blood tests reveal specific patterns that help pinpoint underlying conditions:
| Hormone Pattern Possible Condition High FSH/LH | Ovarian Failure |
| Low FSH/LH | Hypothalamic Issues |
| High Prolactin | Pituitary Problems |
| High Androgens | PCOS |
These hormone measurements guide treatment decisions and help healthcare providers develop targeted therapeutic approaches for women experiencing amenorrhea ICD 10 related conditions.
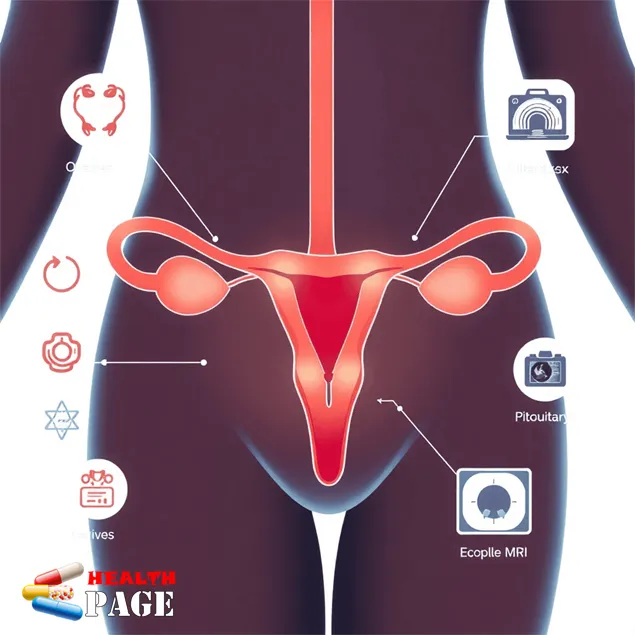
Imaging Studies: A Valuable Tool in Assessing Structural Abnormalities Causing Amenorrhea
Medical imaging plays a vital role in diagnosing structural causes of amenorrhea. Different imaging techniques reveal specific anatomical details:
1. Pelvic Ultrasound
- Visualizes ovarian size and structure
- Detects uterine abnormalities
- Identifies presence of ovarian cysts
- Shows endometrial thickness variations
2. Magnetic Resonance Imaging (MRI)
- Provides detailed views of reproductive organs
- Reveals congenital anomalies
- Detects pituitary tumors
- Shows potential obstructions in the reproductive tract
3. Hysterosalpingography
- Examines fallopian tube patency
- Identifies uterine cavity shape
- Shows potential blockages
- Reveals structural defects
These imaging studies help healthcare providers create targeted treatment plans. Pelvic ultrasound serves as the initial screening tool. MRI offers detailed anatomical information when ultrasound results need clarification. The choice of imaging depends on specific clinical symptoms and suspected underlying conditions.
Learn more about reproductive imaging techniques
Comprehensive Clinical Evaluation and Management Strategies for Women with Amenorrhea
A thorough clinical evaluation for women with amenorrhea requires a systematic approach to identify underlying causes. Medical professionals assess multiple factors:
Key Components of Clinical Evaluation:
- Detailed medical history
- Family history of reproductive disorders
- Medication review
- Lifestyle factors assessment
- Physical examination findings
- Laboratory test results
- Imaging study interpretations
The management strategy varies based on the specific diagnosis:
Primary Amenorrhea Treatment Options:
- Hormone replacement therapy
- Surgical intervention for anatomical abnormalities
- Genetic counseling when appropriate
- Regular monitoring of bone health
Secondary Amenorrhea Interventions:
- Lifestyle modifications
- Weight management programs
- Stress reduction techniques
- Medication adjustments
- Specific treatments for underlying conditions
Healthcare providers create personalized treatment plans considering:
- Patient’s age
- Desire for fertility
- Presence of other health conditions
- Individual preferences
- Available support systems
Regular follow-up appointments help track progress and adjust treatments. Patient education plays a vital role in successful management of amenorrhea ICD 10 conditions. Support groups can provide additional resources and emotional assistance during treatment.
Success rates vary depending on the underlying cause. Early detection through recognition of the 10 alarming signs linked to amenorrhea ICD 10 in women improves treatment outcomes.
FAQs (Frequently Asked Questions)
What is amenorrhea and why is it significant in women’s health?
Amenorrhea refers to the absence of menstruation and is a critical indicator of reproductive health issues in women. Understanding its causes and types helps in early diagnosis and management, ensuring better overall health outcomes.
How does ICD-10 coding assist in diagnosing amenorrhea?
ICD-10 coding, specifically code N91.2 for unspecified amenorrhea, provides a standardized medical classification system that aids healthcare professionals in accurately diagnosing and documenting amenorrhea cases for effective treatment planning.
What are the differences between primary and secondary amenorrhea?
Primary amenorrhea is the absence of menstruation by age 15 or 16 with normal growth and secondary sexual characteristics, often due to genetic or congenital conditions like Müllerian agenesis. Secondary amenorrhea refers to the cessation of menstruation for three months or more in women who previously had regular periods, commonly caused by conditions such as PCOS or hypothalamic-pituitary dysfunction.
Which hormonal disorders are commonly linked to primary amenorrhea?
Hormonal disorders such as androgen insensitivity syndrome play a significant role in causing primary amenorrhea by affecting menstrual function, necessitating specific diagnostic evaluations and targeted management strategies.
How do physical signs like breast development and pubic hair presence assist in identifying underlying causes of amenorrhea?
Assessment of physical signs such as breast development status and presence or absence of pubic hair provides essential clues about hormonal balance and potential underlying conditions associated with amenorrhea, guiding further diagnostic investigations.
What diagnostic tools are utilized to evaluate structural abnormalities causing amenorrhea?
Imaging studies including pelvic ultrasound and magnetic resonance imaging (MRI) are valuable tools used to assess structural abnormalities in reproductive organs that may contribute to amenorrhea, facilitating accurate diagnosis and individualized treatment planning.
