
Latest Update on White Lung Syndrome: Symptoms and Treatments
White lung syndrome has become a significant health concern, especially with the recent increase in pneumonia cases worldwide. This condition, characterized by distinctive white patches visible on chest X-rays, represents a severe form of pneumonia that requires immediate medical attention.
The medical community has noticed a significant rise in cases, particularly among children. This increase has prompted healthcare providers and public health officials to be more vigilant. The pattern of infection suggests that various pathogens, including bacteria, viruses, and fungi, are working together to cause this serious respiratory condition.
Understanding white lung syndrome is crucial for several reasons:
- Early detection can lead to better treatment outcomes
- Proper identification helps healthcare providers choose appropriate interventions
- Awareness enables individuals to seek timely medical care
- Knowledge of preventive measures can reduce transmission risks
The impact of white lung syndrome goes beyond individual health issues; it also has broader public health implications. As cases continue to rise, healthcare systems worldwide are adapting their response strategies. This includes improved monitoring, updated treatment plans, and increased public health messaging to ensure communities stay informed and protected.
The growing prevalence of white lung syndrome highlights the need for a comprehensive understanding of its symptoms, causes, and available treatments. This knowledge empowers both healthcare providers and the public to respond effectively to this respiratory health challenge.
What is White Lung Syndrome?
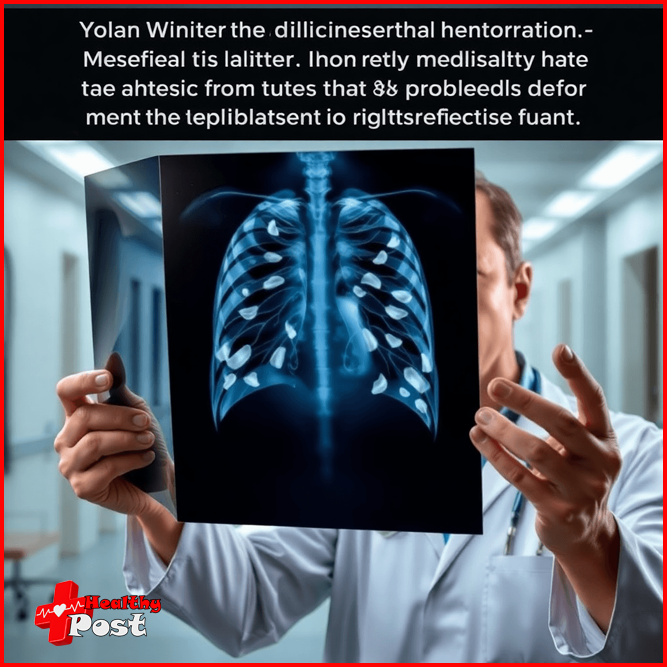
White lung syndrome is a severe form of pneumonia that can be identified by specific white patches seen on chest X-rays. These white areas indicate significant inflammation and fluid buildup in the lung tissue, which contrasts sharply with the normally dark appearance of healthy lung tissue on radiographic images.
How White Lung Syndrome Gets Its Name
The term “white lung” comes from the findings that medical professionals observe during diagnosis. When examining a chest X-ray of an affected patient, doctors look for:
- Dense white areas replacing normal lung tissue
- Bilateral involvement affecting both lungs
- Patchy or widespread white regions indicating infection spread
Assessing Severity Through Imaging
The severity of white lung syndrome can be determined by looking at the extent of white patches visible on imaging:
- Mild cases: Small, localized white areas
- Moderate cases: Multiple patches spread across lung fields
- Severe cases: Extensive white regions throughout both lungs
Differences from Typical Pneumonia Cases
White lung syndrome differs from regular pneumonia cases in several ways:
- Rapid progression
- Extensive lung involvement
- Significant impact on breathing capacity
- Higher risk of complications
Understanding the Radiological Changes
The white appearance on X-rays is caused by various changes happening in the lungs:
- Fluid accumulation in air sacs
- Inflammatory cell infiltration
- Thickening of lung tissue
- Collection of cellular debris
These alterations can severely affect the lungs’ ability to carry out their crucial function of exchanging oxygen, resulting in breathing difficulties and necessitating immediate medical attention.
Causes of White Lung Syndrome
White lung syndrome is caused by various infectious agents that lead to severe inflammation and fluid accumulation in the lungs. These pathogens can be broadly classified into three main categories:
1. Bacterial Infections
- Streptococcus pneumoniae – The most common bacterial cause, responsible for up to 30% of cases
- Mycoplasma pneumoniae – Often seen in younger patients
- Staphylococcus aureus – Can lead to severe cases, particularly in hospitalized patients
- Haemophilus influenzae – Less common due to widespread vaccination
2. Viral Pathogens
- Respiratory Syncytial Virus (RSV) – A leading cause in children under 5
- Influenza viruses – Both Type A and B can trigger severe lung inflammation
- SARS-CoV-2 – The virus responsible for COVID-19 can cause white lung appearance
- Parainfluenza viruses – Common in pediatric cases
3. Fungal Infections
- Aspergillus species – Most frequent fungal cause
- Pneumocystis jirovecii – Primarily affects immunocompromised individuals
- Cryptococcus – Rare but severe cases reported
Several risk factors can increase a person’s susceptibility to developing white lung syndrome:
- Weakened immune system
- Age (very young children and elderly)
- Chronic health conditions
- Recent hospitalization
- Exposure to respiratory pathogens
The severity of white lung syndrome can vary based on several factors:
- Type of pathogen involved
- Patient’s immune status
- Time between symptom onset and treatment initiation
- Presence of any underlying health conditions
Recent data suggests an increase in cases linked to multiple pathogens simultaneously, creating more complex clinical presentations. This phenomenon, known as co-infection, poses additional challenges for treatment and recovery.
Symptoms of White Lung Syndrome
White lung syndrome presents with distinct symptoms that can significantly impact daily activities. Understanding these warning signs helps in early detection and prompt medical intervention.
Primary Symptoms:
- Persistent Wet Cough: Produces thick, colored mucus, often worse in the morning, disrupting sleep patterns and lasting several weeks.
- Respiratory Distress: Shortness of breath during routine activities, rapid breathing (tachypnea), difficulty completing sentences, and chest tightness or pain.
- Fever and Related Symptoms: High temperature (typically 101°F/38.3°C or higher), body aches and chills, night sweats, and cold-like symptoms.
Impact on Daily Activities:
- Physical Limitations: Reduced ability to exercise or climb stairs, difficulty carrying out household chores, limited mobility due to fatigue, and decreased appetite affecting energy levels.
- Sleep Disruption: Nighttime coughing fits, difficulty lying flat, frequent awakening due to breathing issues, and need for elevated head position during sleep.
Additional Warning Signs:
- Bluish tint to lips or fingernails
- Rapid heart rate
- Mental confusion or disorientation
- Severe fatigue affecting concentration
- Loss of appetite leading to weakness
- Nausea or vomiting
Children may show additional symptoms such as:
- Irritability
- Decreased feeding
- Grunting sounds while breathing
- Nostril flaring during respiration
- Retractions (visible pulling of chest muscles during breathing)
These symptoms can vary in severity from person to person, with some experiencing mild discomfort while others require immediate medical attention. The intensity often depends on factors such as age, overall health status, and the underlying cause of the infection.

Diagnosis Methods for White Lung Syndrome
Medical professionals use various diagnostic tools to effectively identify and evaluate white lung syndrome. The diagnosis process usually starts with a physical examination and review of medical history, followed by specific imaging tests.
Primary Diagnostic Tools:
- Chest X-rays: These imaging tests reveal characteristic white patches in lung tissue, show fluid accumulation patterns, help determine the extent of lung involvement, and enable tracking of disease progression.
- CT Scans: CT scans provide detailed 3D images of lung tissue, identify subtle changes missed by X-rays, show precise location and distribution of inflammation, and assist in detecting complications.
Laboratory Tests:
- Mucus Sample Analysis: This test identifies specific pathogens causing infection, determines whether the origin is bacterial, viral, or fungal, guides appropriate treatment selection, and helps monitor antibiotic resistance.
Additional Diagnostic Procedures:
- Blood Tests: These tests include a complete blood count to check infection levels, blood culture to identify bloodstream infections, measures inflammation markers, and assesses organ function.
- Pulse Oximetry: This procedure monitors blood oxygen levels, helps determine severity, and guides oxygen therapy needs.
Medical professionals often combine these diagnostic methods to create a comprehensive picture of the patient’s condition. The results help determine the most effective treatment approach and monitor recovery progress. Early and accurate diagnosis plays a crucial role in managing white lung syndrome effectively and preventing potential complications.
In severe cases where standard diagnostic methods prove inconclusive, healthcare providers may also perform bronchoscopy. This procedure allows direct visualization of the airways and collection of deeper tissue samples for further analysis.
Treatment Options for White Lung Syndrome Based on Cause
The treatment strategy for white lung syndrome varies significantly based on the underlying pathogen causing the infection. Medical professionals tailor specific approaches depending on whether bacteria, viruses, or fungi are responsible for the condition.
Bacterial Infections
- Broad-spectrum antibiotics serve as the primary treatment
- Common prescriptions include:
- Amoxicillin
- Azithromycin
- Clarithromycin
- Treatment duration typically spans 7-14 days
- Doctors may adjust antibiotics based on culture results
Viral Infections
- Antiviral medications prescribed for specific viral strains
- Treatment options include:
- Oseltamivir for influenza
- Ribavirin for RSV in severe cases
- Medication timing crucial – most effective when started early
Fungal Infections
- Antifungal medications required for extended periods
- Treatment options include:
- Voriconazole
- Amphotericin B
- Duration may extend several weeks to months
Hospitalization Requirements
- Severe cases need intensive care monitoring
- Treatment may include:
- Oxygen therapy
- Intravenous (IV) medications
- Respiratory support
- Close monitoring of vital signs and oxygen levels
Medication Administration
- Routes vary based on severity:
- Oral medications for mild cases
- IV treatments for severe infections
- Nebulized medications for direct lung delivery
- Regular assessment of treatment response through imaging and clinical symptoms
Medical professionals carefully monitor patients’ responses to treatment, adjusting medications as needed based on clinical improvement and potential side effects. The recovery timeline varies significantly among patients, influenced by factors such as age, underlying health conditions, and the specific pathogen involved.
Supportive Care and Home Remedies for Symptom Relief in White Lung Syndrome Patients
While medical treatments target the underlying infection, supportive care plays a vital role in managing symptoms and speeding up recovery for white lung syndrome patients. Here are essential supportive measures patients can implement at home:
Rest and Sleep
- Maintain extended periods of uninterrupted rest
- Keep your head elevated while sleeping to ease breathing
- Create a quiet, comfortable environment for quality sleep
Hydration and Nutrition
- Drink 8-10 glasses of water daily
- Consume warm liquids like herbal tea or broth
- Eat small, nutrient-rich meals focusing on:
- Protein-rich foods
- Fresh fruits and vegetables
- Whole grains
Breathing Support
- Use a humidifier to add moisture to the air
- Practice deep breathing exercises when comfortable
- Maintain an upright sitting position during the day
Natural Symptom Relief
- Apply warm compresses to chest area
- Try honey for cough suppression
- Use salt water gargle for sore throat
- Take steamy showers to loosen mucus
Environmental Considerations
- Keep room temperature moderate
- Ensure good air circulation
- Avoid exposure to irritants like:
- Smoke
- Strong fragrances
- Dust
- Pet dander
Activity Management
- Start with gentle movements as strength returns
- Listen to your body’s signals
- Gradually increase activity levels
- Take frequent breaks during daily tasks
These supportive measures complement prescribed medical treatments and help create optimal conditions for recovery. Patients should maintain regular communication with healthcare providers and report any worsening symptoms or concerns during the recovery process.
Preventive Measures Against White Lung Syndrome Infections Through Vaccination and Hygiene Practices
Protection against white lung syndrome starts with a robust vaccination strategy. The Centers for Disease Control and Prevention (CDC) recommends two essential vaccines:
Key Vaccinations:
- Pneumococcal vaccine – Guards against Streptococcus pneumoniae bacteria
- Annual flu shot – Reduces risk of influenza-related pneumonia
These vaccines create a defensive shield, significantly lowering the chances of developing severe respiratory infections that could lead to white lung syndrome.
Essential Hygiene Practices
- Wash hands with soap for 20 seconds
- Use alcohol-based sanitizers when soap isn’t available
- Cover mouth and nose when coughing or sneezing
- Dispose of used tissues immediately
- Clean frequently touched surfaces daily
Environmental Controls
- Maintain proper ventilation in indoor spaces
- Use air purifiers with HEPA filters
- Keep humidity levels between 30-50%
- Avoid exposure to secondhand smoke
Lifestyle Modifications
- Get adequate sleep (7-9 hours)
- Stay physically active
- Maintain a balanced diet rich in vitamins C and D
- Quit smoking or avoid exposure to tobacco smoke
- Stay hydrated with 8-10 glasses of water daily
High-Risk Groups Need Extra Precautions
- Children under 5 years
- Adults over 65
- People with compromised immune systems
- Those with chronic respiratory conditions
Workplace and school settings require additional preventive measures:
- Regular sanitization of shared spaces
- Implementation of sick leave policies
- Proper spacing between workstations
- Encouraging remote work/learning during illness
These prevention strategies work best when implemented consistently and combined with regular health check-ups and prompt medical attention at the first sign of respiratory symptoms.
Latest Updates on Cases and Research Regarding White Lung Syndrome Globally
Recent data from global health organizations reveals a significant increase in white lung syndrome cases across multiple regions. China reported a notable surge in pediatric pneumonia cases during November-December 2023, with hospitals experiencing increased patient admissions.
Key Statistics from Recent Studies:
- Denmark documented a 150% rise in mycoplasma pneumonia cases compared to previous years
- The Netherlands recorded an 80% increase in pediatric pneumonia hospitalizations
- Ohio (USA) reported a cluster of 145 pediatric cases between August-December 2023
Research teams at major medical institutions have identified several emerging patterns:
- A shift in pathogen behavior, with some bacterial strains showing enhanced resistance to traditional treatments
- Higher transmission rates among school-aged children (5-14 years)
- Seasonal variations affecting case numbers, with peak occurrences during winter months
Regional Distribution of Cases:
- Asia Pacific: Concentrated outbreaks in China, South Korea, and Vietnam
- Europe: Scattered clusters across multiple countries, with higher rates in Northern regions
- North America: Localized surges in specific states and provinces
Current research focuses on understanding the factors behind these increased cases. Scientists at the World Health Organization are investigating potential mutations in common respiratory pathogens and their role in disease severity. Preliminary findings suggest environmental factors and post-pandemic immune system responses may contribute to the rising numbers.
The medical community continues to monitor case patterns through enhanced surveillance systems, with particular attention to pediatric cases and treatment outcomes. This data helps healthcare providers adjust treatment protocols and resource allocation strategies.
Community Awareness Initiatives Promoting Understanding About White Lung Syndrome Amongst Public Health Campaigns
Public health organizations worldwide have launched targeted campaigns to educate communities about white lung syndrome. These initiatives focus on early recognition of symptoms and preventive measures through:
Digital Education Programs
- Interactive webinars hosted by healthcare professionals
- Social media campaigns with shareable infographics
- Virtual support groups for affected families
- Mobile apps tracking respiratory symptoms
Community Outreach
- School-based health education programs
- Local clinic information sessions
- Multilingual educational materials
- Door-to-door awareness campaigns in high-risk areas
Healthcare Provider Training
- Updated diagnostic guidelines for medical professionals
- Specialized workshops on treatment protocols
- Resource distribution to rural healthcare centers
- Telemedicine support networks
The CDC and WHO have created dedicated web portals providing:
Real-time updates on case numbers Treatment guidelines Prevention strategies Resources for healthcare providers
Local health departments have implemented rapid response teams to:
- Monitor community spread
- Provide immediate medical guidance
- Coordinate with schools and daycare centers
- Distribute educational materials
These initiatives emphasize practical prevention methods through:
- Hand hygiene demonstrations
- Proper mask-wearing techniques
- Vaccination awareness
- Environmental cleaning protocols
The success of these campaigns relies on community participation and consistent messaging across all platforms. Health authorities continue to adapt their strategies based on new research and changing patterns in disease spread.
FAQs (Frequently Asked Questions)
What is white lung syndrome?
White lung syndrome is a severe form of pneumonia characterized by distinct features visible on chest X-rays. Infected areas appear white due to fluid accumulation, indicating significant respiratory illness.
What are the common causes of white lung syndrome?
White lung syndrome can be caused by various pathogens including bacteria such as Streptococcus pneumoniae, viruses like influenza and respiratory syncytial virus (RSV), and less commonly, fungal infections such as aspergillosis.
What symptoms are associated with white lung syndrome?
Common symptoms include a wet cough, fever, and shortness of breath. These symptoms can be severe and significantly impact daily activities.
How is white lung syndrome diagnosed?
Diagnosis primarily involves imaging tests such as chest X-rays and CT scans to visualize characteristic findings. Analyzing mucus samples from the lungs is also crucial for identifying the specific pathogen causing the infection.
What treatment options are available for white lung syndrome?
Treatment depends on the underlying cause of the infection. Antibiotics are used for bacterial cases, while antiviral medications may be prescribed for viral infections. Fungal infections require specific antifungal treatments.
What preventive measures can be taken against white lung syndrome?
Preventive measures include getting vaccinated against influenza and pneumococcal bacteria, as well as practicing good hygiene to reduce the risk of developing severe pneumonia with a white lung manifestation.
