
Stem cells – the new power to restore light
If God gave you three days of light, where would you most like your eyes to stay? The famous American writer Helen Keller answered this in her book “If You Give Me Three Days of Light”. I will definitely let my eyes stay on the things I cherish. So that I can recall them one by one in the darkness of the future. What a helpless choice this is, tragic and desolate… Now, with the development of bioscience and technology. Stem cells have opened a new chapter in the treatment of eye diseases.
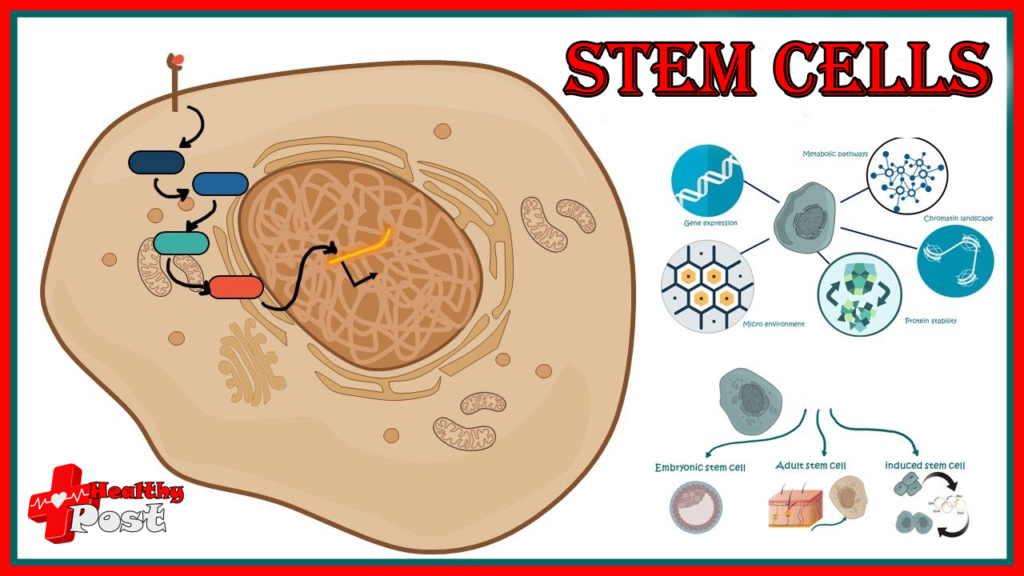
Modern treatments for different eye diseases are evolving rapidly. In recent years, ophthalmologists have devoted a lot of attention to stem cell research. At present, stem cells have made great progress in the treatment of many kinds of eye diseases.
1. Myopia
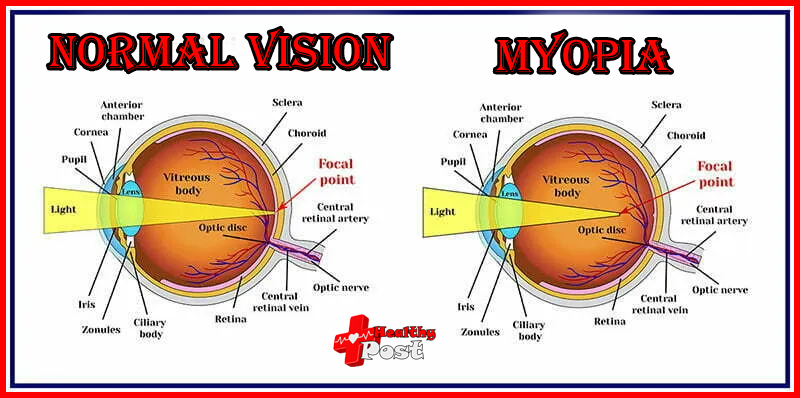
With the development of science and technology, the ubiquity of TVs, mobile phones and tablets has enriched. The field of vision and greatly reduced people’s time for outdoor activities. Data released by the National Health Commission in July 2021 showed that in 2020,
The age at which myopia occurs is getting younger, and there are more and more people with high myopia. Effective treatments are urgently needed to prevent the development of childhood myopia and reduce the incidence of myopia.
Mesenchymal stem cells have been successfully use in a variety of clinical applications for connective tissue regeneration/reconstruction. The properties of mesenchymal stem cells make them ideal candidate cells for scleral reinforcement. Since the pathological mechanism of the development of myopia is consistent with the characteristics of stem cells, subscleral injection of mesenchymal stem cells can strengthen the originally fragile sclera of myopic patients. The transplanted cells are expected to differentiate into fibroblasts and produce extracellular matrix. Strengthen the sclera and prevent the eyeball from elongating, thus preventing or preventing myopia (Figure 2).
Note the elongation of the axial length of the eye and the thinning of the sclera over time. As well as the prospect of halting disease progression with early treatment.
These include combining injected mesenchymal stem cells with direct mechanical support of the scleral structure. As well as indirect stimulation of the scleral tissue through the production of dopamine, thereby preventing eye elongation.
2. Retinitis pigmentosa
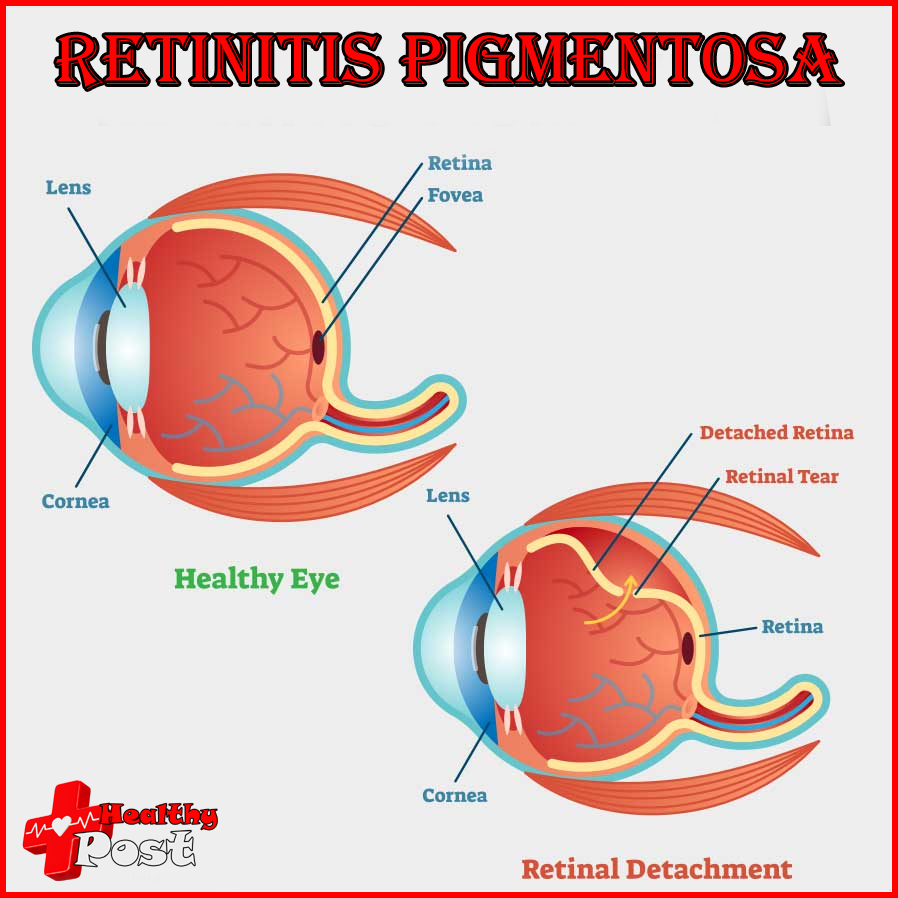
This Retinitis pigmentosa (RP) is a group of inherited eye diseases that result in progressive loss of vision due to damage and eventual death of retinal cells. Since the optic nerve and retinal ganglion cells do not have the ability to regenerate, they will cause irreversible damage after being damaged and undergoing apoptosis.
The main mechanism of action of mesenchymal stem cells in degenerative diseases is to regulate. The microenvironment with paracrine effects by secreting growth factors. They can serve as a source of nutritional factors, promote cell survival and activate intrinsic repair mechanisms. Because MSC do not express major histocompatibility complex (MHC) on the cell surface. This advantage allows autologous or allogeneic use without the risk of rejection. After transplantation, patients do not need to receive any immunosuppressive treatment to prevent rejection.
In the Phase 3 clinical trial published on the “Research Gate” website, experienced surgeons used the Limoli retinal repair technology (LRRT) under local anesthesia. Limoli et al. described this [5-7], injecting a stem cell suspension into the adipose tissue between the transplanted choroid and sclera. During the surgery, each eye received 5 million UC-MSCs, and A six-month follow-up observation was conducted.
In 2010, the US company ACT (advanced cell technology) received FDA approval to use embryonic stem cell-derived retinal pigment epithelial cells (RPE) to treat two degenerative eye diseases: dry age-related macular degeneration (Dry age-related macular degeneration, AMD) and juvenile macular dystrophy (Stargardt disease). This is the second FDA-approved clinical trial involving human embryonic stem (hES) cells.
Research institution
In 2012, the research institution published an article “Embryonic stem cell trials for macular degeneration: a preliminary report” in The Lancet magazine [9]. US researchers used human embryonic stem cells (hESC) to treat two patients with different degenerative eye diseases. Early data shows that hESC treatment is not only safe but also shows some therapeutic efficacy. They induced hESCs to generate early bone cells and neural tissue cells, which then differentiated into retinal epithelial cells with a purity of over 99%.
The researchers injected approximately 50,000 isolated retinal epithelial cells into the subretina of two patients, an elderly female patient who developed dry age-related macular degeneration in her 70s and another who was The young female patient suffered from Stargardt disease, which resulted in both blindness. Four months later, the researchers found that the RPE had been completely replaced by the injected retinal epithelial cells. The data confirmed that the injected cells survived and greatly improved their vision. (as shown in the table)
3. Macular degeneration
Macular degeneration is usually a natural result of age-related degeneration. As age increases, the retinal tissue degenerates and becomes thinner, causing a decline in macular function. Macular degeneration is divided into two types: age-related macular degeneration and juvenile macular degeneration. Age-related macular degeneration (ARMD) has been increasing in incidence over the past few decades. It is one of the leading causes of blindness in people over the age of 60.
The disease characterized by macular degeneration is the loss of retinal pigment epithelial cells (RPE), which in turn causes degenerative changes in photoreceptor cells (cones, rods), etc.; the patient gradually loses visual acuity and is unable to read, read newspapers or drive. travel. However, current clinical treatments cannot eradicate the cause, and some patients respond poorly to treatment. As a result, new treatments for macular degeneration have begun to be explored. Stem cell therapy replaces dying RPE cells in patients, saving eyes before vision loss occurs.
RPE can be differentiated from human embryonic stem cells (hESCs) or human induced pluripotent stem cells (iPSCs) [12-14]. Before the photoreceptor is irreversibly damaged, RPE cells differentiated from stem cells are used to replenish the lost or degenerated RPE cells. The differentiated cells have a similar morphology to the RPE cells, can express RPE markers, and have the ability to phagocytose the outer segments of the photoreceptor.
Nature Biotechnology
An article [16] published in Nature Biotechnology describes a stem cell-derived retinal pigment epithelial patch that can be used to treat sudden severe blindness caused by macular degeneration. The researchers used specially designed microsurgical tools to implant the patch into the subretinal space of one eye of two patients with severe exudative macular degeneration. The retinal pigment epithelial patch was successfully implant through biomicroscopy and optical coherence tomography and survived. Twelve months after the surgery, the two patients’ visual acuity improved by 29 and 21 words respectively (Figure 5). This clinical study provides evidence for the feasibility and safety of human embryonic stem cell RPE patch transplantation as a treatment for age-related macular degeneration.
(a) Patient 1 had best-corrected visual acuity for more than 12 months.
(b) Patient 1’s reading speed exceeds 12 months.
(c) Patient 2 has had best corrected visual acuity for more than 12 months.
(d) Reading speed of patient 2 over 12 months.
4. Glaucoma
Glaucoma is a neurodegenerative disease, the pathological features of which are optic nerve atrophy and visual field loss, which lead to visual impairment and vision loss, and in severe cases, blindness. The pathogenic mechanism is pathological increase in intraocular pressure and insufficient blood supply to the optic nerve.
The current treatment methods are to reduce intraocular pressure and perform optic nerve protection treatment through drugs or surgery. These methods can only play a certain protective role, but cannot fundamentally prevent optic nerve damage.
Some researchers have used mesenchymal stem cells to treat animal optic nerve injury models and found that the therapeutic effect is obvious. The mechanism is that the homing mesenchymal stem cells secrete cytokines through paracrine action to repair damaged nerve cells.
In 2013, Stem Cells magazine published an article “Transplantation of Mesenchymal Stem Cells Promotes TissueRegeneration in a Glaucoma Model Through Laser-Induced Paracrine FactorSecretion and Progenitor Cell Recruitment”.
Researchers from Canada transplanted mesenchymal stem cells into glaucoma models, which can promote glaucoma tissue regeneration through laser-induced paracrine factor secretion and progenitor cell proliferation. Experiments show that mesenchymal stem cells in bone marrow induce the regeneration of trabecular meshwork cells, and injection into the anterior chamber of the eye is more effective than hematopoietic cells in causing a decrease in intraocular pressure (IOP) (p<0.001) (Figure 6). In addition, mesenchymal stem cells and the factors they secrete induce reactivation of the progenitor cell pool in the ciliary body and promote cell proliferation.
Laser-induced tissue
Laser-induced tissue remodeling introduces mesenchymal stem cells into the damaged area according to the predetermined target, and also causes a certain increase in eye progenitor cells. This study demonstrates that mesenchymal stem cells and their secreted components are key mediators of tissue repair via local neural progenitor cells in open-angle glaucoma.
(A): 1×106 bone marrow mononuclear cells (red), 1×106 lymphocytes (black), and normal saline (green) were inject into the anterior chamber without additional treatment (blue). The gray area indicates the normal range of intraocular pressure. Intraocular pressure is report as the mean ± SEM of four experiments, with 12 animals evaluated per group.
(B): 0.5×106 T cells (black) or 0.5×106 mesenchymal stem cells (red) were inject intraocularly after laser irradiation and evaluated as above. The means ± SEM of three experiments with 9 animals per group were evaluate.
5. Cataract
Cataract refers to the clouding of the lens in the eye, which changes from transparent to opaque, blocking light from entering the eye, thus affecting vision. In the early stage, when the cloudiness is mild or small in scope, it does not affect vision, but then gradually worsens to significantly affect vision or even cause blindness. The vision loss caused by cataracts cannot be correct by wearing glasses. The World Health Organization estimates that about 20 million people in the world are blind by cataracts, making it the world’s number one blinding eye disease.
Traditional treatment methods usually use ultrasound to soften and break the lens, flushing it out, and then the doctor implants an artificial lens in the patient’s eye. However, severe inflammation and complications may occur after surgery, and may even lead to irreversible blindness. Intraocular lenses are not only expensive, but also do not have the ability to be sensitive and precise in physiological adjustment. Glare symptoms often occur after surgery, which affects visual quality [19]. These inherent drawbacks of intraocular lenses have prompted the search for new cataract treatments.
A team led by Professor Liu Yizhi from the Sun Yat-sen University Ophthalmology Center discovered that endogenous stem cells exist on the lens of the eyeball, and used these stem cells to regenerate a transparent lens in situ. It was the first time to achieve the regeneration of solid tissues and organs with physiological functions in the human body. In clinical treatment of congenital cataract. The findings were publish in the journal Nature in March 2016. In the experiment, 12 children with congenital cataracts under the age of 2 underwent this new surgical method, which regenerated functional lenses and reduced the recurrence rate by more than 20 times.
Clinical trial
This clinical trial confirmed the new surgical method in the treatment of congenital cataracts. The safety and effectiveness in cataracts provide a new strategy for cataract treatment and open up a new direction for tissue regeneration and clinical application of stem cells.
In addition, transplantation of limbal stem cells, oral mucosal epithelial cells, corneal epithelial stem cells, etc. to treat corneal damage; embryonic-derived pigment epithelial cells (ES derived RPE) and Research on hematopoietic stem cell and mesenchymal stem cell transplantation to treat some eye lesions caused by autoimmunity is also in full swing.
Scientific researchers around the world have never stopped chasing the bright future. They believe that in the near future, stem cells will be able to cure more eye diseases. It bring light to patients with eye diseases.

