
What is esophageal reflux (GERD)? Symptoms and prevention
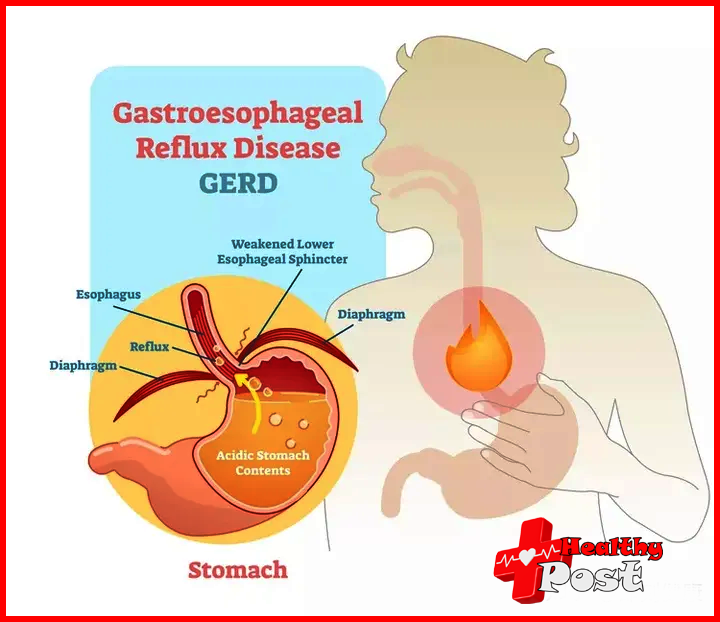
Gastroesophageal reflux disease (GERD) is a gastrointestinal disorder that occurs when stomach acid repeatedly backs up into the esophagus (the tube that carries food from the mouth to the stomach). This can cause symptoms such as heartburn, chest pain, and reflux into the mouth; however, some people experience no symptoms.
Although gastroesophageal reflux disease is usually a chronic, lifelong condition, it can be controlled through lifestyle changes, medications, and, in severe cases, surgery. If you are diagnosed with gastroesophageal reflux disease, you must make medication and lifestyle changes as prescribed by your doctor. Doing so can help reduce symptoms and improve quality of life.
Types of esophageal reflux
Gastroesophageal reflux disease is divided into three different types based on the amount of damage it causes to the esophagus. The three different types include non-erosive reflux disease (NERD), erosive esophagitis, and Barrett’s esophagus.
Non-erosive Reflux Disease (NERD)
Non-erosive reflux disease is a type of gastroesophageal reflux disease in which the esophagus is not damage by stomach acid. It is the most common form of gastroesophageal reflux disease, with 60%-70% of patients experiencing it. Non-gastroesophageal reflux may eventually progress to a more aggressive disease. If left untreated, non-GERD can negatively impact the health of your entire digestive system.
erosive esophagitis
Thirty percent of people with gastroesophageal reflux disease develop erosive esophagitis, which occurs when stomach acid refluxes into the throat, causing inflammation or damage to the lining of the esophagus (esophageal mucosa). If left untreated, esophagitis can develop into a condition called Barrett’s esophagus and increase the risk of esophageal cancer.
Barrett’s esophagus
Barrett’s esophagus occurs in 6% to 12% of patients with gastroesophageal reflux. This condition occurs when the tissue lining the esophagus is replaced by tissue similar to the lining of the intestine. This is a severe form of gastroesophageal reflux disease that can lead to a rare cancer called esophageal adenocarcinoma.
Symptoms of gastroesophageal reflux disease
A band of muscle called the lower esophageal sphincter works with the diaphragm to prevent stomach contents from refluxing into the esophagus. If this barrier relaxes at the wrong time or becomes damaged in some way, you can develop gastroesophageal reflux disease.
Symptoms of gastroesophageal reflux disease can begin after repeated or long-term exposure to stomach acid. But it’s important to note that not everyone develops GERD in the same way, and it’s possible to have no symptoms at all. Potential symptoms of gastroesophageal reflux disease include
- Heartburn
- reflux of gastric contents
- chest pain
- Dysphagia (dysphagia)
- chronic cough
- hoarse voice
- unexplained weight loss
Sometimes people experience what is call a lump in the throat, or a lump in the throat that interferes with swallowing.
What is the cause of gastroesophageal reflux disease?
Technically, the cause of gastroesophageal reflux disease is unknown; however, researchers have found some possible solutions
One possible explanation is abnormal movement in the digestive system. Esophageal dyskinesia is when the muscles of the digestive system do not work properly and there are changes in the speed, strength or coordination of the body’s digestive organs. This can make it difficult for our bodies to clear the acid from our esophagus.
Another possibility is that the tone of the lower esophageal sphincter is chronically relax, leaving it open and making acid reflux more likely to occur.
Medical experts also speculate that gastroparesis or delayed gastric emptying may be a cause of gastroesophageal reflux disease. Gastroparesis occurs when the digestive system slows down and takes longer for the stomach and small intestine to expel its contents.

risk factors
Certain conditions and anatomic factors increase the risk of developing gastroesophageal reflux disease. For example, if you have a hiatal hernia or have elevated intra-abdominal pressure, your risk of developing gastroesophageal reflux disease is increased. Other risk factors for gastroesophageal reflux disease include a high-fat diet, smoking, and alcohol consumption .
You are also at greater risk of developing gastroesophageal reflux disease if you are pregnant or taking certain medications. For example, 40%-85% of pregnant women develop gastroesophageal reflux, which is likely related to relaxation of the lower esophageal sphincter due to an increase in progesterone, an important reproductive hormone. Meanwhile, the drugs most commonly associated with GERD are nonsteroidal anti-inflammatory drugs (NSAIDs), antibiotics such as tetracyclines and lincomycin, and statins.
diagnosis
Doctors may make a preliminary diagnosis based on symptoms, especially typical symptoms. In this case, they may have the patient try a drug called a proton pump inhibitor (PPI) to see if symptoms improve.
If you have unusual or atypical symptoms, such as difficulty swallowing or unexpected weight loss, your doctor may prescribe tests.
Esophageal pH monitoring
By measuring the pH of a substance, you can learn how acidic or alkaline it is. During esophageal pH monitoring, a small tube with a pH sensor on the tip is passed through the nose into the esophagus. Measurements of acid exposure in the esophagus were collected over 24 hours. This checks how much acid has entered the esophagus.
Typically, your doctor will order this test if you are not sure whether your symptoms are related to GERD or if you are not responding to prescribed medications.
upper endoscopy
This test is do with an endoscope, a small camera attach to a tube that is pass through the mouth into the esophagus. This test allows the doctor to see the lining of the patient’s esophagus and small intestine and, if necessary, take a biopsy (tissue sample).
This invasive test is use when a patient exhibits alarm symptoms such as difficulty swallowing, is unresponsive to PPI medications, or is at high risk for developing Barrett’s esophagus. However, test results are inconclusive; 40%-60% of patients with gastroesophageal reflux have normal test results.
Esophageal manometry
This test requires physical anesthesia and then passing a small tube through the nose into the esophagus. Once the tube is in place, the patient is ask to swallow so that esophageal function and the lower esophageal sphincter can be measure. Although this test does not diagnose gastroesophageal reflux disease, it can give your doctor an idea of how well your esophagus and lower esophageal sphincter are working.
Esophageal Impedance pH Study
Although this test is not widely available, it functions similarly to the 24-hour pH monitoring test. It can also be use when the 24-hour pH probe test results are normal.
A tube is insert through the nose into the esophagus at the level of the lower esophageal sphincter. This test measures the flow of fluid from the stomach to the esophagus. It usually detects bile reflux, not acid reflux. Bile is a digestive fluid made by the liver and stored in the gallbladder.
Esophagography
An esophagogram, sometimes call a barium swallow, is use to evaluate dysphagia (or dysphagia) and is not usually use to diagnose gastroesophageal reflux disease due to its low sensitivity. Instead, this test is use primarily to evaluate hernias and intestinal motility disorders.
Home treatments for gastroesophageal reflux disease
Gastroesophageal reflux disease is a chronic disease that does not resolve on its own and has no cure. Long-term treatment and management are often require. These treatments often include lifestyle changes, medications, and sometimes surgery.
Remember, over-the-counter medications only temporarily relieve symptoms and do not prevent symptoms from returning. They also do not allow an injured esophagus to heal. Here are just a few home treatments for gastroesophageal reflux disease.
change lifestyle
Many doctors will recommend lifestyle changes to reduce symptoms. This may include not smoking, losing weight, and changing your eating habits . They may also recommend elevating the head of the bed to help prevent nighttime gastroesophageal reflux disease and improve sleep hygiene. Sleep reduces transient lower esophageal sphincter relaxation, thereby reducing gastroesophageal reflux symptoms. Wearing loose-fitting clothing may also help.
prevention
While some GERD may be due to age or body structure and function, there are other ways to prevent the possibility of developing GERD. For example, you are more likely to develop gastroesophageal reflux disease if you have a high body mass index (BMI), smoke, or are inactive.
Taking steps to quit smoking or remove secondhand smoke from your home is the first step in preventing GERD . In fact, a 2016 study found that nearly 44 percent of ex-smokers had fewer episodes of gastroesophageal reflux disease one year after quitting.
Controlling your weight can also help prevent gastroesophageal reflux disease, which occurs in a significant proportion of people with a high body mass index (BMI).
Also try incorporating moderate physical activity into your daily habits. Research shows that consistent exercise can help prevent gastroesophageal reflux disease and reduce the likelihood of symptoms if you’re already diagnose with the disease. However, strenuous exercise may aggravate the condition in people who are susceptible to GERD, so you should experiment with what level of exercise is best for you.

Complications of gastroesophageal reflux
Gastroesophageal reflux disease often occurs at the same time as other diseases and may even lead to the development of some diseases. For example, studies show that people with gastroesophageal reflux disease are more likely to wake up during the night and may even experience sleep disturbances. People with gastroesophageal reflux disease are more likely to experience insomnia, sleep dissatisfaction, difficulty falling asleep, and major depression.
A 2017 study found that anxiety and depression were significantly more common among people with gastroesophageal reflux disease. As many as 42% of people with psychological disorders develop gastroesophageal reflux disease, but it is unclear which psychological disorder causes another, or whether there is an inverse relationship between them. Having psychological comorbidities also reduces the likelihood of remission of gastroesophageal reflux symptoms.
Other complications of gastroesophageal reflux include high blood pressure, high cholesterol, and type 2 diabetes .
How to prevent esophageal reflux in daily life?
If you have been diagnose with gastroesophageal reflux disease, it is important to follow your doctor’s instructions, especially if your doctor prescribes medications or recommends lifestyle changes (such as quitting smoking, weight loss, and physical activity). Beyond this, there are other things you can do to reduce symptoms and relieve discomfort.
For example, there is evidence that changing your diet may help. Limit your intake of highly acidic or spicy foods, alcohol, and unhealthy fats as much as possible, and make sure you eat plenty of fruits and vegetables, lean proteins, and healthy fats.
You can try chewing gum to increase saliva production and reduce the amount of acid in your esophagus. Also make sure you have good posture, especially after eating. Try not to lie down for two hours after eating; instead, stand, move around and sit up straight. If gastroesophageal reflux occurs at night, elevating the head of the bed can help.


One thought on “What is esophageal reflux (GERD)? Symptoms and prevention”