How i knew i had colon cancer
How i knew i had colon cancer ? This is an important question. In this article we will explain about everything about colon cancer. Life has a way of throwing unexpected curveballs. At 38, I never imagined I’d be sharing my story about colon cancer. Yet here I am, hoping my experience might help others recognize the signs I initially dismissed.
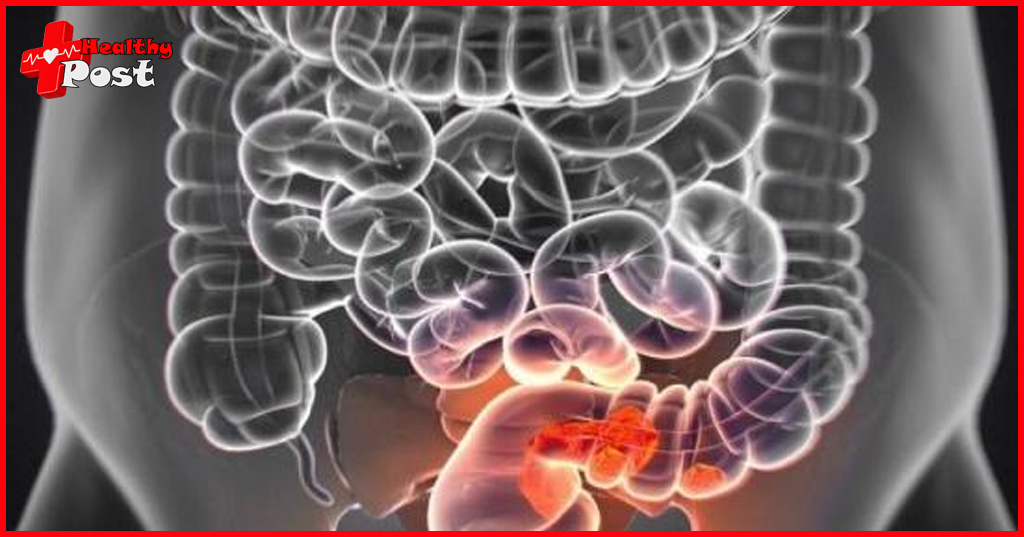
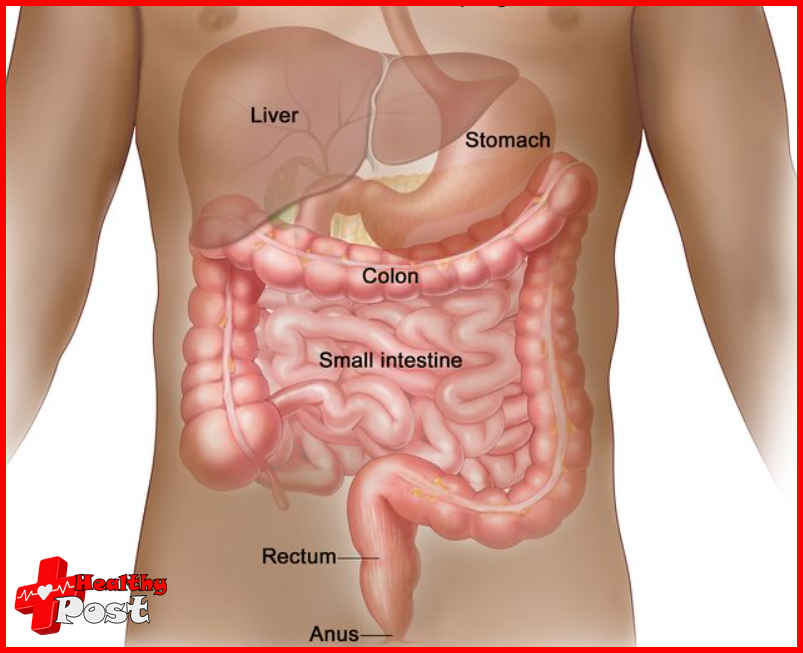
Colon cancer starts in the large intestine (colon), the final part of our digestive tract. It’s a silent invader that often develops from small, harmless clumps of cells called polyps. These polyps can become cancerous over time – a process that might take years without showing any symptoms.
I learned this the hard way. Looking back, the signs were there, but like many others, I brushed them off as stress-related digestive issues. That’s the tricky thing about colon cancer – its symptoms can masquerade as everyday health problems.
Why Early Detection Matters:
- Colon cancer is highly treatable when caught early
- The 5-year survival rate for localized colon cancer is 90%
- Treatment options are more effective in earlier stages
- Recovery tends to be faster with early intervention
My journey began with subtle changes in my body that I couldn’t quite explain. As a busy professional and parent, it was tempting to ignore these warning signs. Now I know that listening to our bodies and acting on concerns isn’t being paranoid – it’s being proactive about our health.
Recognizing the Signs: My Initial Symptoms
Looking back, I can see that the signs were there months before I was diagnosed. It started with subtle changes in my bowel habits – occasional constipation followed by unexplained diarrhea. I dismissed these symptoms as stress-related or dietary issues, trying to convince myself it was nothing serious.
The first warning sign appeared when I noticed blood in my stool. At first, it was just tiny streaks, barely noticeable. I rationalized it as hemorrhoids, a common explanation I’d found during late-night Google searches. The bleeding became more frequent, and bright red spots would appear on the toilet paper.
My body was trying to tell me something:
- Persistent abdominal cramps that felt different from regular stomach aches
- Unexplained fatigue that coffee couldn’t fix
- A constant feeling of incomplete bowel movements
- Sudden weight loss without changing my diet or exercise routine
The most concerning symptom was the intense abdominal pain that would wake me up at night. It started as a dull ache on my lower left side and gradually got worse. These weren’t normal stomach cramps – they felt deeper, more persistent, and wouldn’t go away with over-the-counter medications.
I spent weeks trying to brush off these symptoms, blaming them on poor eating habits or work stress. Each morning, I’d wake up hoping the symptoms would go away, but they only got stronger.
Navigating Misdiagnoses: The Struggle for Answers
My journey through the healthcare system felt like running in circles. When I first shared my symptoms with my primary care physician, they quickly labeled it as IBS. “It’s just stress-related,” they said, prescribing antispasmodics and suggesting dietary changes.
For six months, I followed their advice religiously. I eliminated trigger foods, practiced stress management, and took my medications. Yet my symptoms persisted – the cramping grew worse, and the blood in my stool became more frequent.
The IBS diagnosis didn’t sit right with me. My body was trying to tell me something more serious was happening, but medical professionals kept dismissing my concerns. Each doctor’s visit ended with the same response: “IBS can cause these symptoms.”
I started documenting everything – my symptoms, their frequency, and severity. This detailed log became my voice when doctors wouldn’t listen. It was frustrating to know something was wrong while being told repeatedly that it was “just IBS.”
Looking back, those months of misdiagnosis could have cost me dearly. My case isn’t unique – many colon cancer patients initially receive an IBS diagnosis due to overlapping symptoms.
The Turning Point: Seeking Medical Help
I reached my breaking point during a family dinner. I couldn’t ignore the stabbing pain in my abdomen anymore – it felt different from the usual discomfort. The blood in my stool had become more frequent, and I’d lost 15 pounds without trying. My sister noticed my pale complexion and how I barely touched my food.
That night, I lay awake scrolling through medical websites, comparing my symptoms. Each search pointed to something more serious than IBS. The next morning, I called my primary care physician’s office, insisting on an immediate appointment.
This time, I documented every symptom in detail:
- Unexplained weight loss
- Dark blood in stool
- Severe abdominal pain
- Constant fatigue
- Loss of appetite
I refused to leave the doctor’s office without a referral for additional testing. Something inside me knew – this wasn’t just IBS acting up. My body was trying to tell me something, and I needed answers.
The Importance of Specialized Care: Consulting a Gastroenterologist
My primary care doctor’s referral to a gastroenterologist marked a critical turning point in my diagnosis journey. The gastroenterologist’s specialized knowledge and expertise in digestive system disorders brought a new level of understanding to my symptoms.
During my first appointment, I noticed the difference in approach. The gastroenterologist asked detailed questions about my symptoms, family history, and lifestyle – things I hadn’t discussed with other healthcare providers. She explained that persistent changes in bowel habits, combined with my other symptoms, warranted immediate investigation.
The specialist ordered specific tests:
- A colonoscopy to examine my colon
- Blood work to check for anemia and other markers
- CT scan to get detailed images of my digestive system
What struck me most was her thorough explanation of each test’s purpose. She didn’t dismiss my concerns or attribute them to stress, unlike previous experiences. Her expertise in identifying subtle warning signs proved invaluable.
The gastroenterologist’s role extended beyond ordering tests. She created a comprehensive plan to investigate my symptoms systematically. Her specialized training in digestive system disorders meant she knew exactly what to look for and which tests would provide the most accurate information.
Looking back, consulting a gastroenterologist was the decisive step that led to my accurate diagnosis. Their specialized knowledge can make the difference between early detection and delayed treatment. This experience underscored the importance of seeking specialized care when faced with complex health issues, as illustrated in this article.
Facing the Reality: Receiving My Colon Cancer Diagnosis
The words hit me hard. “I’m sorry, but the tests confirm you have stage 4 colon cancer.” Time seemed to freeze as I tried to comprehend what I had just heard. The doctor’s voice sounded far away as she went over the details of the colonoscopy and showed me the pictures on her computer.
My wife held my hand tightly, tears streaming down her face. I felt numb, struggling to understand what this meant for me and my family. The doctor pointed out the large tumor that had been causing my symptoms all along. Questions flooded my mind: How long do I have? What will happen to my children? Can I still work?
The diagnosis process included:
- Multiple blood tests
- CT scans of my abdomen
- A colonoscopy revealing the tumor
- Tissue biopsies confirming malignancy
That day changed everything. The diagnosis explained my persistent symptoms, but it also marked the beginning of a challenging journey. My doctor’s calm demeanor and clear explanation of the next steps helped ground me during those overwhelming moments.
Understanding My Diagnosis: Staging and Prognosis Explained
After the initial shock of my diagnosis, my oncologist walked me through the staging process. The medical team used a combination of tests to determine my cancer’s stage:
- CT scans revealed the size of my tumor and any spread
- Blood tests measured specific markers like CEA levels
- Tissue samples from my colonoscopy helped analyze the cancer cells
My stage 4 diagnosis meant the cancer had spread beyond my colon to other organs. The staging system runs from 1 to 4:
- Stage 1: Cancer in the colon’s inner layers
- Stage 2: Cancer has grown into the colon wall
- Stage 3: Cancer has reached nearby lymph nodes
- Stage 4: Cancer has spread to distant organs
The prognosis discussion was challenging but necessary. My doctor explained survival rates vary significantly based on multiple factors:
- Age and overall health
- Specific genetic mutations
- Response to treatment
- Location of metastases
Understanding these details helped me grasp the complexity of my condition and prepared me for the treatment decisions ahead. My medical team emphasized that statistics are general guidelines, not individual predictions. Each person’s cancer journey is unique, and modern treatments offer new possibilities for extending life and improving quality of life.
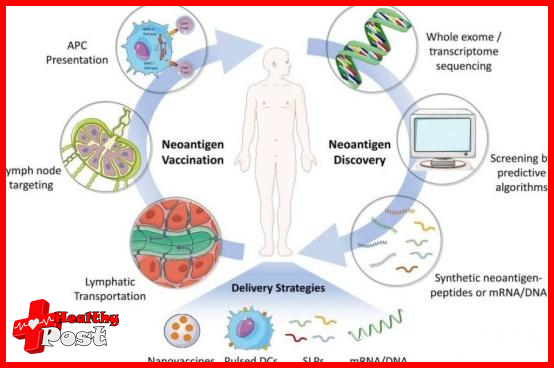
Exploring Treatment Options: A Personal Perspective
After my diagnosis, I sat down with my oncology team to discuss treatment choices. The path ahead seemed daunting, but understanding my options helped me feel more in control.
My treatment plan included three main components:
- Surgery: A right hemicolectomy to remove the tumor and surrounding tissue
- Chemotherapy: FOLFOX protocol administered every two weeks
- Targeted therapy: Specific medications designed to attack cancer cells
The surgery was scheduled first. My surgeon explained they would remove about 12 inches of my colon where the tumor had grown. I remember feeling scared but also relieved knowing we had a concrete plan of action.
Chemotherapy started six weeks after my surgery. I received treatments through a port – a small device implanted under my skin. Each session lasted about four hours. The medical team monitored my progress closely, adjusting medications when needed to manage side effects.
I also explored complementary therapies:
- Acupuncture for nausea relief
- Nutritional counseling to maintain strength
- Gentle yoga classes designed for cancer patients
Making these treatment decisions wasn’t easy. I researched extensively, asked countless questions, and relied heavily on my medical team’s expertise. Each choice felt personal, tailored to my specific situation and needs. The journey taught me there’s rarely a one-size-fits-all approach to cancer treatment.
Coping with the Challenges: Side Effects and Support Systems
The reality of cancer treatment hit me hard when the side effects began. My body felt like it was fighting a constant battle – not just against cancer, but against the treatments meant to save my life.
Physical Challenges I Faced:
- Intense nausea that made eating feel impossible
- Debilitating fatigue that kept me in bed for days
- Hand-foot syndrome that made simple tasks painful
- Hair loss that changed how I saw myself in the mirror
My support system became my lifeline during these difficult moments. My spouse took charge of meal preparations, creating small, nutrient-rich portions I could manage. Friends organized a rotation schedule to drive me to appointments when fatigue overwhelmed me.
I discovered unexpected comfort in online support groups. Connecting with others who understood exactly what I was experiencing provided validation and practical tips. One group member suggested freezing coconut water into ice chips – a simple trick that helped me stay hydrated through the worst bouts of nausea.
Working with my medical team, we developed strategies to manage side effects:
- Taking anti-nausea medications before symptoms peaked
- Gentle walking when energy allowed
- Moisturizing routines for skin care
- Modified diet plans based on my changing needs
The hospital’s social worker connected me with local resources, including a cancer support center offering free counseling sessions. These conversations helped me process the emotional weight of treatment while learning new coping mechanisms.
Fortunately, there are numerous cancer support services available that provide invaluable assistance during such challenging times. For instance, CancerCare offers a variety of resources including counseling and support groups which can be incredibly beneficial. Additionally, organizations like the American Cancer Society provide extensive support programs tailored to individual needs. Furthermore, exploring options like those provided by the UCSF Health Patient and Family Cancer Support Center can also offer much-needed help in navigating this difficult journey.
Advocating for Awareness: The Need for Early Detection and Screening
My diagnosis at age 35 opened my eyes to a startling reality – colon cancer isn’t just an “old person’s disease.” The rising cases among young adults under 50 paint a concerning picture. Recent statistics show approximately 19,000 new cases annually in the U.S. among younger individuals.
I’ve made it my mission to share my story, especially with younger people who might dismiss early warning signs. The misconception that age protects us from colon cancer can be deadly. Many of my fellow survivors discovered their diagnosis at advanced stages due to delayed screenings.
Here’s what everyone needs to know about screening:
- The recommended age for initial screening has dropped to 45
- High-risk individuals should start earlier
- Family history plays a crucial role in determining screening schedules
- Regular screenings can detect polyps before they become cancerous
Through social media and local support groups, I connect with others to spread awareness. I emphasize the importance of listening to your body and advocating for proper medical attention. My experience taught me that early detection dramatically impacts survival rates.
Young adults need to understand their risk factors and recognize potential symptoms. A simple screening could have caught my cancer at an earlier stage. Now, I dedicate time to educating others about these life-saving tests and encouraging open discussions about digestive health.
My Message to Others: Hope, Resilience, and Taking Action Against Colon Cancer
Living with colon cancer has changed how I see life. Every day comes with its own set of difficulties, but it also offers chances to grow and bounce back. I’ve come to understand that being diagnosed with cancer doesn’t determine your identity – it’s your reaction that influences your path.
To anyone going through similar struggles, keep these in mind:
- Trust your instincts: Your body sends signals when something isn’t right. Listen to these messages and act on them
- Be your own advocate: Push for answers when you feel dismissed or misunderstood by healthcare providers
- Embrace support: Let family and friends help you through difficult times
- Take it day by day: Some days will be harder than others, and that’s okay
My fight against colon cancer showed me what true strength is. I found bravery within me that I never knew existed. The road ahead may look scary, but remember, you’re not alone on this journey.
“Hope is like the sun. If you only believe in it when you can see it, you’ll never make it through the night.”
I encourage you to stay updated, ask for help when necessary, and always hold onto hope. Your experiences are important, and your struggle makes an impact. Together, we can spread the word and support one another during this tough time.
Remember – early detection saves lives. Don’t hesitate to take action. Your health needs immediate care, and you deserve the best treatment available.
FAQs (Frequently Asked Questions)
What are the early symptoms of colon cancer?
Common early symptoms of colon cancer include bloody stools and abdominal pain. It’s important to pay attention to these signs and consult a healthcare professional if you experience them.
Why is early detection crucial for colon cancer?
Early detection of colon cancer is crucial because it significantly increases the chances of successful treatment. The earlier the cancer is diagnosed, the more options are available for effective intervention.
What should I do if I suspect I have colon cancer?
If you suspect you have colon cancer due to concerning symptoms, it’s essential to seek medical attention promptly. A healthcare provider can evaluate your symptoms and recommend appropriate diagnostic tests.
How can a gastroenterologist help in diagnosing colon cancer?
A gastroenterologist specializes in digestive system disorders and plays a critical role in diagnosing colon cancer. They can perform necessary examinations, such as colonoscopies, to identify any abnormalities in the colon.
What treatment options are available for colon cancer?
Treatment options for colon cancer may include surgery to remove tumors, chemotherapy to target cancer cells, and radiation therapy. The specific approach depends on the stage of the disease and individual patient factors.
How can I cope with the side effects of colon cancer treatment?
Coping with treatment side effects involves managing symptoms through medication, dietary changes, and support from healthcare professionals and loved ones. It’s important to communicate openly with your medical team about any challenges you face during treatment.