Difficulty with neurological examination? Learn to master them easily in 6 steps.
Neurological examination is one of the most important basic skills for neurologists. Reliable neurological signs provide crucial evidence for clinical diagnosis, but novice neurologists are often overwhelmed by the complexity and tediousness of neurological examinations . This article summarizes the experiences and insights of Professor Chen Shengyun, Director of the Emergency Department and Chief Physician of the Department of Cerebrovascular Medicine at Sanbo Brain Hospital, Capital Medical University, during his clinical teaching.
Step 1: Examination of level of consciousness, speech, and mental state
The state of consciousness refers to the central nervous system’s ability to respond to stimuli from the internal and external environment, including the level and content of consciousness. Its examination can locate a wide range of the cerebral cortex and the ascending reticular activating system in the brainstem.
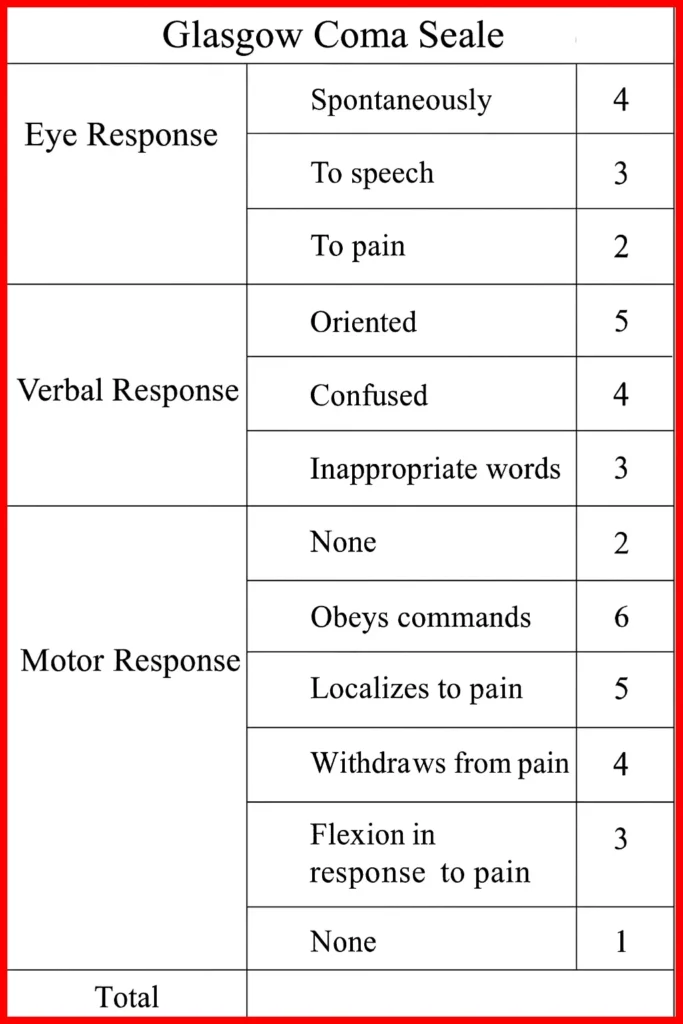
The level of consciousness is assessed as: drowsy, confused, stuporous, and comatose (mild, moderate, and severe). The specific state can be determined by referring to the Glasgow Coma Scale.
Step 2: Cranial nerve examination
There are 12 pairs of cranial nerves in total. The key points of examination include ptosis (III), facial drooping or asymmetry (VII), clarity of speech (V, VII, X, XII), abnormal eye position (III, IV, VI), and abnormal or asymmetrical pupils (II, III).
In addition, the sensitivity of the sense of smell, visual acuity and visual field, fundus examination, hearing examination, palpebral fissure, changes in voice, morphology and strength of related muscles, and eye movements should also be included in the examination.
Step 3: Musculoskeletal system examination
The examination of the musculoskeletal system mainly consists of six parts: muscle strength, muscle tone, muscle volume, coordination, involuntary movements, posture, and gait.
In principle, assessing muscle strength requires the patient to perform an action against external resistance, comparing both sides, and generally using a six-level grading system of 0-5.
- Grade 0: No muscle contraction, no joint movement, indicating complete paralysis;
- Grade 1: The muscles contract slightly, but cannot move the joints.
- Level 2: Muscle contraction can drive joint movement, but cannot counteract the weight of the limb;
- Level 3: Able to resist the gravity of the limbs, but unable to resist resistance;
- Level 4: Able to partially resist resistance and allow the joint to move, but the joint is not stable;
- Level 5: Able to resist resistance, with normal muscle strength and stable joints.
Muscle tone usually refers to the tension of muscles at rest. Intracranial lesions can cause abnormal muscle tone . When examining muscle volume, three points should be noted: hypertrophy, atrophy, and symmetry. Coordination tests mainly include the finger-to-nose test, rapid alternating movements, heel-to-shin test, and the sign of difficulty standing with eyes closed.
Step 4: Sensory System Check
Before each sensory system examination, the contents and questions of the examination should be clearly explained to the patient. Unless under specific circumstances, the patient should keep their eyes closed during the examination. Special attention should be paid to whether the two sides of the body are symmetrical during the examination, and the distal and proximal parts of the limbs should be compared. If a sensory loss area is found, its boundaries should be described in detail.
The senses tested include superficial senses (pain, temperature, touch), deep senses (kinesthetic sense, position sense, vibration sense), and complex senses (solid sense, graphic sense, two-point discrimination).
Step 5: Reflection Inspection
One important point to note when examining reflexes is that they need to be checked in conjunction with motor function. Reflexes mainly include superficial reflexes (corneal reflex, abdominal wall reflex, cremasteric reflex, anal reflex, plantar reflex ), deep reflexes (biceps brachii reflex, triceps brachii reflex, radial periosteal reflex , ankle reflex, knee reflex), and pathological reflexes. Different reflexes correspond to different nerves.
Step 6: Examination of pathological reflexes and abnormal gait –
In clinical practice, we often encounter patients with a neutral Babinski sign. In such cases, it is necessary to conduct further examinations of other Babinski sign equivalents to determine the specific situation. Commonly used equivalents include Chaddock sign, Oppenheim sign , Gordon sign, Gonda sign, and Pussep sign. Abnormalities in different equivalents represent different types of nerve damage.
In addition, there are other pathological reflex examinations. Such as Brucella sign, Korgny sign, sucking reflex, meningeal irritation sign, and neck stiffness.
Gait changes are a common manifestation of nerve damage. All patients who can walk should have their gait examined. Common types include spastic hemiplegic gait, spastic paraplegic gait , ataxia gait , panicked gait, straddling gait, swaying gait, and drunken gait.


One thought on “Difficulty with neurological examination? Learn to master them easily in 6 steps.”